How is the drug name pronounced?
Phesgo: FES-goh
Pertuzumab: per-TOO-zoo-mab
Trastuzumab: trass-TOO-zoo-mab
Hyaluronidase: hye-al-yoor-ON-i-dase
What cancer(s) does this drug treat?
Early breast cancer
Phesgo is approved for:
- Patients with breast cancer that has spread within the breast or to the lymph nodes under the arms, but not to other parts of the body; is inflammatory or early stage; and tests positive for high amounts of the HER2 molecule. In such cases, Phesgo is used in combination with chemotherapy before surgical removal of all known disease.
- Patients with breast cancer that tests positive for high amounts of the HER2 molecule, and who are at high risk for their cancer coming back after surgical removal of all known disease.
Advanced breast cancer
Phesgo is approved for:
- Patients with breast cancer that tests positive for high amounts of the HER2 molecule and has spread to other parts of the body, and who have not received prior treatments that target the HER2 molecule, or chemotherapy for their advanced disease. In such cases, Phesgo is used in combination with docetaxel chemotherapy.
Limitations of Use
Age: The safety and efficacy of Phesgo in patients under 18 years of age have not been established.
Pregnancy/Breastfeeding: Treatment with Phesgo can cause harm to a fetus, and is not recommended for use during pregnancy. Women are advised to use contraception during treatment with Phesgo and for at least 7 months after the last dose of Phesgo. The risks associated with Phesgo during breastfeeding are not known and cannot be ruled out. Due to the potential for reactions in the breastfed child, the benefits of breastfeeding and the mother’s need for treatment should be weighed accordingly before moving forward with treatment with Phesgo.
Hypersensitivity: Phesgo should not be administered to patients who have had allergic reactions to pertuzumab (Perjeta), trastuzumab (e.g., Herceptin), hyaluronidase, or any other compounds of Phesgo in the past.
What type of immunotherapy is this?
- Cell-killing antibody
How does this drug work?
- Target: Human epidermal growth factor receptor 2 (HER2)
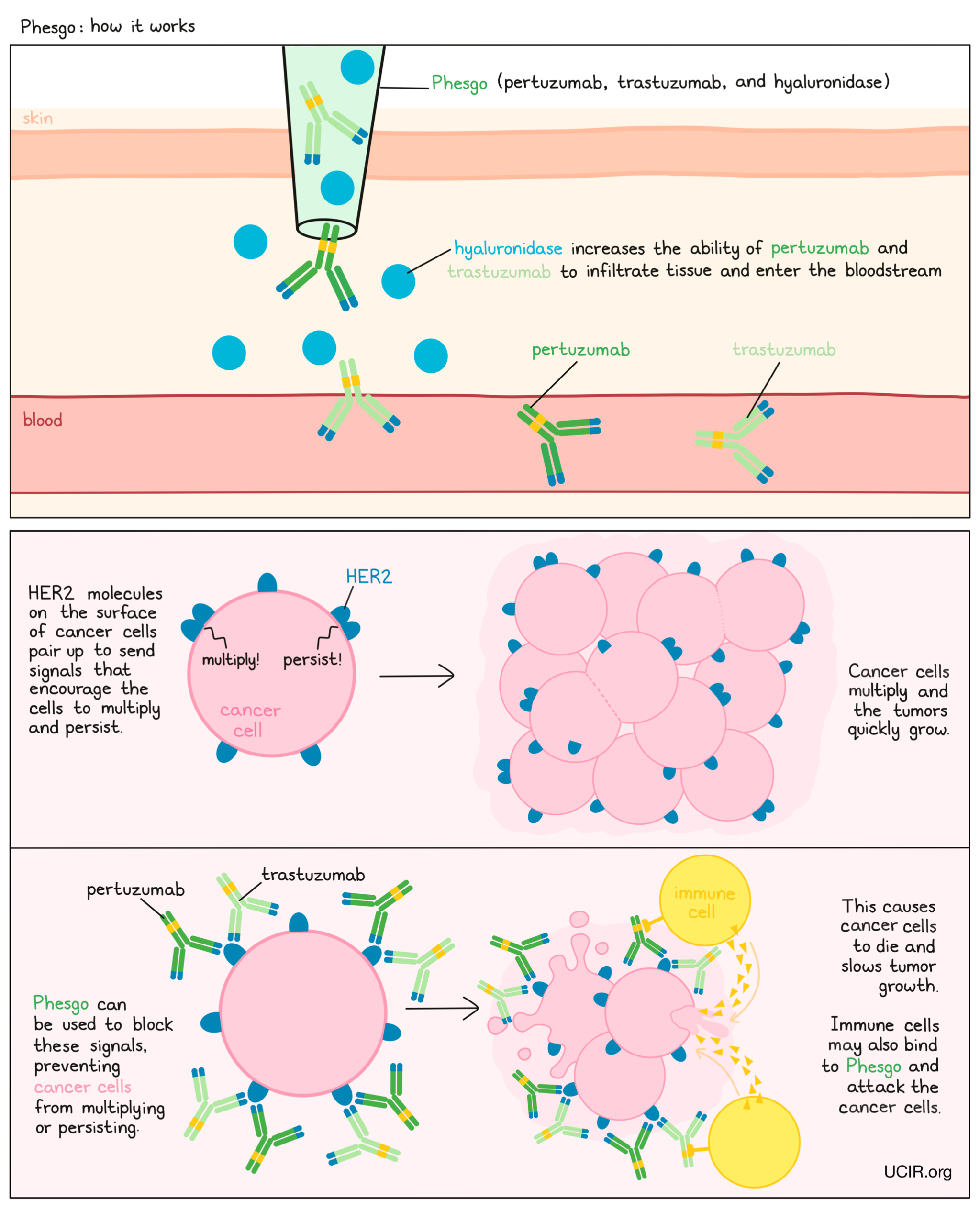
Phesgo is a combination treatment of pertuzumab (Perjeta), trastuzumab (e.g., Herceptin), and hyaluronidase. Pertuzumab and trastuzumab are the therapeutic components of the treatment, while hyaluronidase is added to increase the ability of pertuzumab and trastuzumab to infiltrate into tissue under the skin and enter the bloodstream.
Pertuzumab and trastuzumab are antibodies that were made in the laboratory and were designed to attach to a protein molecule called HER2. HER2 is present on the surface of some normal cells in the body, and is also present in much higher quantities on the surface of breast cancer cells. Higher-than-normal amounts of HER2 on cancer cells make these cells the main targets of pertuzumab and trastuzumab. Pertuzumab and trastuzumab bind the HER2 molecule on different sides. When administered together, both drugs can achieve a greater benefit than pertuzumab or trastuzumab alone.
Pertuzumab, trastuzumab, and other antibody molecules have an overall “Y” shape. The two tips of the upper arms of the “Y” shape are the parts of the antibody that can very precisely bind to their targets. Both pertuzumab and trastuzumab attach to HER2. The stems of pertuzumab’s and trastuzumab’s “Y” shapes can attract immune cells or other parts of the immune system.
Phesgo works to kill cancer cells in at least two ways:
Cancer cell growth inhibition and cancer cell death
When HER2 on the surface of cells binds to itself or to other HER2-related proteins, it sends signals into the cell. These signals cause the cell to multiply and persist. Higher-than-normal amounts of HER2 allow cancer cells to grow and multiply out of control. Binding of pertuzumab and trastuzumab to HER2 blocks HER2 from pairing up and sending these signals into the cancer cells, preventing the cells from persisting and multiplying, and forcing HER2-positive breast cancer cells to undergo “programmed cell death”.
Antibody-dependent cell-mediated cytotoxicity (ADCC)
When bound to HER2 on the surface of breast cancer cells, the stem of pertuzumab or trastuzumab can also attract and bind immune cells. This allows pertuzumab and trastuzumab to act as a bridge between the target cell and an immune cell (such as a natural killer (NK) cell). The immune cell then releases molecules that can kill the cell that pertuzumab and/or trastuzumab is bound to.
How is this drug given to the patient?
Before starting treatment with Phesgo, a small tumor sample is collected from a patient and tested to determine if the tumor tests positive for high amounts of the HER2 molecule. Patients also undergo a thorough assessment of the condition of their heart before starting treatment and during treatment with Phesgo.
Phesgo is administered in the form of an injection under the skin (subcutaneous [s.c.] injection) of the thigh and does not require a hospital stay. Patients receive a higher initial dose of Phesgo, administered over about 8 minutes, followed by lower “maintenance” doses given every 3 weeks over approximately 5 minutes. Patients are observed for 15 to 30 minutes after Phesgo injection to monitor for unwanted reactions to the injection. Pheso is given before administration of the chemotherapy.
When given as a treatment for early breast cancer, patients receive 3 to 6 doses of Phesgo at the 3-week interval before complete surgical removal of all known disease and continue treatment after surgery to complete a full year of therapy, or until disease progresses and gets worse or the side effects become unmanageable. Patients with advanced breast cancer are treated with Pheso every 3 weeks until the disease progresses and gets worse or the side effects become unmanageable.
Patients who are currently treated with pertuzumab (Perjeta) and trastuzumab (e.g., Herceptin), which are administered through a tube in the vein (intravenous infusion), can switch treatment to Phesgo (or vice versa).
What are the observed clinical results?
It is important to keep in mind that each patient’s actual outcome is individual and may be different from the results found in the clinical studies. In addition, with immunotherapy, sometimes it takes several months for responses to be observed.
In a clinical trial, 500 patients with breast cancer that had spread within the breast or to the lymph nodes under the arms, but not to other parts of the body or was inflammatory, and tested positive for high amounts of the HER2 molecule, were either treated with Phesgo, or with pertuzumab (Perjeta) and trastuzumab (e.g., Herceptin), which were administered through a tube in the vein (intravenous infusion) before and after surgical removal of all known disease, together with chemotherapy. Both treatments resulted in a similar benefit, with 60% of patients seeing their cancer disappear entirely.
In another clinical trial, 160 patients with breast cancer that tested positive for high amounts of the HER2 molecule, were treated with 3 doses of Phesgo and 3 doses of pertuzumab (Perjeta) and trastuzumab (e.g., Herceptin), which were administered through a tube in the vein (intravenous infusion) at a 3-week interval to prevent the cancer from coming back after surgical removal of all known disease. After having received all 6 doses, all 160 patients completed a questionnaire:
- 85% of the patients reported preferring injection of Phesgo under the skin over infusion of pertuzumab and trastuzumab into a vein. The most common reason was that administration required less time in the clinic.
- 14% of the patients reported preferring infusion of pertuzumab and trastuzumab over Phesgo. The most common reason was that they felt more comfortable during administration.
- 1% of the patients had no preference for the route of administration.
What are the potential side effects?
The most common side effects of Phesgo in combination with chemotherapy include hair loss, rash, nausea, diarrhea, fatigue, weakness, nerve damage (tingling, numbness, or pain in hands and feet), low red blood cell count, and low white blood cell count.
Some side effects, such as heart problems, lung problems, and hypersensitivity reactions can become serious or life-threatening. Patients and caregivers receive careful instructions to monitor for signs and symptoms related to these conditions. These conditions are managed by the healthcare provider.
Heart problems
Phesgo can cause heart problems, including high blood pressure, uneven heartbeat, dysfunction of the heart’s left ventricle, heart disease, heart failure, and heart attack. Prior to the initiation of treatment with Phesgo, patients undergo a thorough assessment of the condition of their heart. Patients also have their hearts monitored regularly during treatment with Phesgo, and have their treatment discontinued if severe heart issues occur.
Lung problems
Treatment with Phesgo can damage the lungs, resulting in inflammation of the lung, excessive fluid in the lungs, buildup of fluid around the lungs, scarring of the lungs, or respiratory failure. Symptoms of these conditions include difficulty breathing, pain while breathing, chest pain, coughing, fatigue, or a feeling of drowning (especially when lying down). A healthcare provider should be immediately notified if symptoms occur.
Hypersensitivity reactions
Hypersensitivity reactions are allergic reactions caused by the body’s immune system responding to Phesgo as if it were a threat. Symptoms of a hypersensitivity reaction may include rashes, itching, wheezing, swelling of the face, shortness of breath, swelling of the airways, and anaphylactic shock.
Patients should report any symptoms to their healthcare provider, who can then initiate actions to limit or reverse the side effects. For a more complete list of possible side effects, see the full prescribing information.
Additional Information
Manufacturer
Genentech/Roche
Approval
FDA and EMA
Website
Last updated on January 26, 2022


