Immunology 101 - Lesson 4
The cancer immunity cycle
The immune system is the human body’s natural defense system. While it is best known for fighting infections and threats that come from outside of the body, it also plays a key role in managing threats from within – like cancer. Cancer arises when mutations in normal cells cause them to thrive and multiply out of control, ignoring the body’s signals to stop, and often forming solid masses or tumors. Mutations in cancer cells may also cause them to behave irregularly, often producing abnormal or out-of-place molecules called antigens, which the immune system can recognize as potentially dangerous. When immune cells patrolling the body find and recognize evidence of cancer, they initiate a multi-step coordinated attack to eliminate it and stimulate further immune control as needed. This process acts as a continuous, repetitive loop, commonly referred to as the cancer immunity cycle.
The cancer immunity cycle starts with the detection of the cancerous cells. As cancer cells grow and divide, some also die, releasing antigens and “danger signals” – molecules or patterns that tell the immune system that something has been damaged or that something is wrong. These danger signals will catch the attention of any patrolling immune cells, which will begin to repair and clean up the area, picking up cellular debris, including the antigens. Some of these immune cells will be antigen-presenting cells – a group that includes dendritic cells, macrophages, and others – and will pick up the antigens, engulf (“eat”) them, break them down (“digest” them), and then display fragments of the antigens on their cell surface so that other immune cells can recognize them.
Once the antigen-presenting cells are loaded up with antigens, they travel to nearby lymph nodes, where T cells (the warriors of the immune system) lie in wait. The antigen-presenting cells then fulfill their function of “presenting” the antigens to the T cells, and if any of the T cells recognize the antigens, they will begin to activate. While recognition of an antigen serves as the first “go” signal, T cells need additional signals from their environment before they can become fully activated and launch an attack. To nudge the T cell further into action, antigen-presenting cells provide additional signals using molecules on their surface called CD80 and CD86 to trigger activation “buttons” called CD28 on the T cell surface. Antigen-presenting cells may also release cytokines, which act as additional “go” signals to stimulate the T cells. Once a T cell receives enough “go” signals, it will become activated enough to begin to multiply, forming an army of T cells that will be sent out into the body in search of any cells that contain the antigen they are programmed to recognize.
Once T cells arrive at the site of a tumor, they must infiltrate it and make contact with the cancer cells. If the cancer cells contain the antigen that the T cells are programmed to recognize, the T cells will launch a strong attack against the cancerous cells. As the cancer cells die, they release more antigens and danger signals that draw the attention of more antigen-presenting cells, and thus, the cancer immunity cycle begins again.

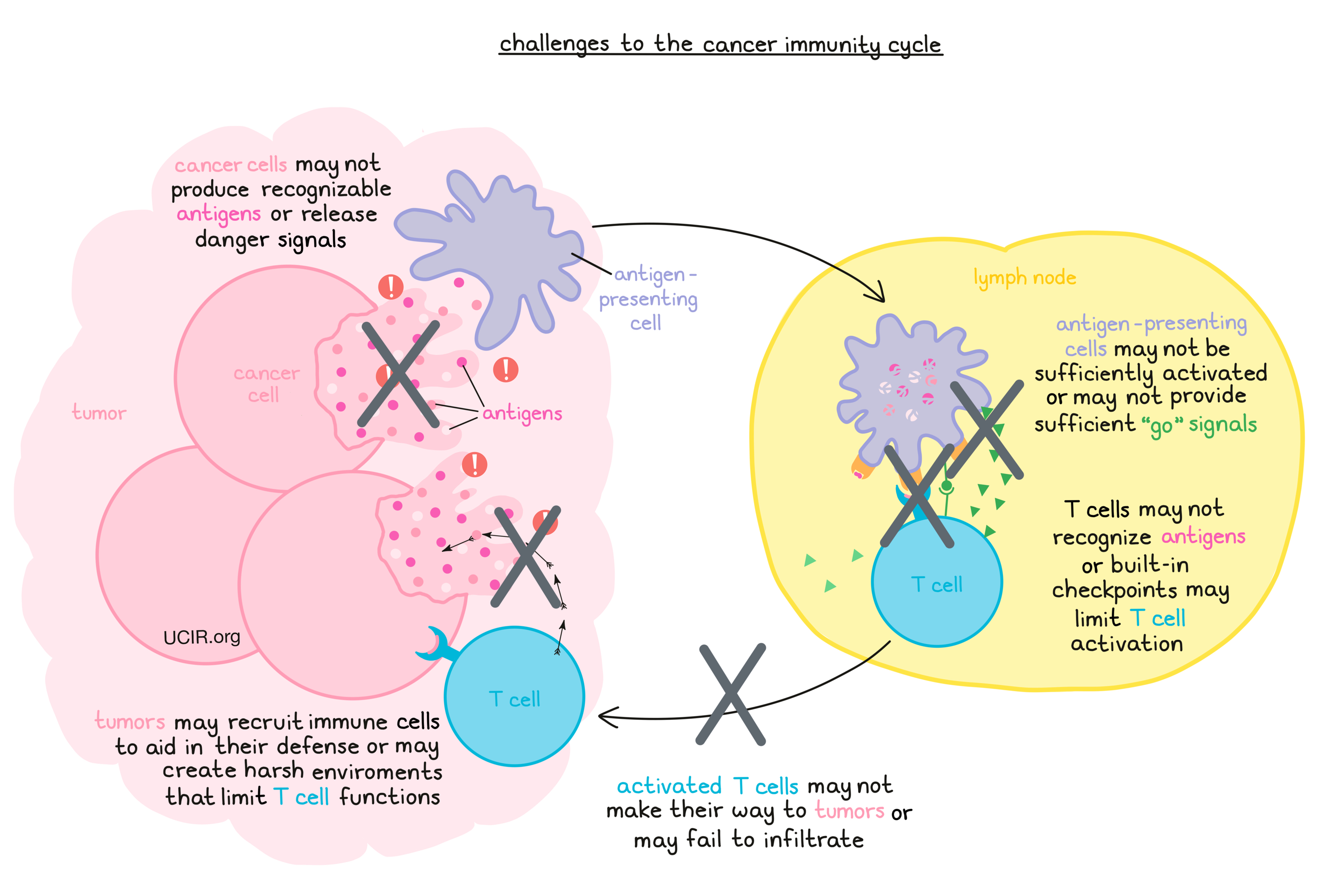
Challenges to the cancer immunity cycle
The immune system plays an important role in detecting and protecting the body against cancer and abnormal cells with the potential to cause cancer. In fact, many of these cells are likely caught and killed by the immune system well before any serious problems occur. However, cancer cells that slip past this system of “immune surveillance” can be highly adaptable, and may find ways to further evade or defend against the immune system. When a patient is diagnosed with cancer, it means that the cancer escaped the immune system’s control, and that the cancer immunity cycle was insufficient, interrupted, or blocked.
There are many points during the cancer immunity cycle where immunity can fall short, allowing the cancer to continue to grow. This can be due to built-in regulatory systems that keep the immune system from responding too strongly and harming healthy tissue, or due to defense mechanisms set up by the cancer. For example, cancer cells often closely resemble normal cells, so some or all of the cancer cells in a particular tumor may not produce any unfamiliar molecules (antigens) that are strongly recognized by the immune system. Similarly, the cancer cells may not produce enough “danger signals” when they die, allowing them to remain unnoticed. At the antigen presentation phase, antigen-presenting cells may not be activated enough, and may not provide sufficient “go” signals to the T cells to induce a strong response. T cells themselves also contain “checkpoints” – built-in systems that prevent overactivation and unwanted attacks against healthy tissues. However, these checkpoints can also minimize wanted activation, limiting the functions of T cells with the potential to recognize and eliminate cancer cells. Activated T cells may also fail to make their way to tumors, or may fail to infiltrate them due to the defensive systems of the tumor, which often make the tumor environment inhospitable for T cells. Even T cells that do manage to make their way into tumors may be limited by the harsh environment within the tumor or by other immune cells that the tumor has recruited to aid in its defense. Tumors may also take advantage of other T cell checkpoints to inactivate T cells that have already infiltrated, and suppress their tumor-killing functions. Finally, even when T cells launch a successful attack against the antigens they are programmed to target, not all cancer cells are the same, and some cancer cells that do not contain the antigen may still be able to escape from the T cell attack and go on to thrive.
Enhancing the cancer immunity cycle
Most forms of cancer immunotherapy involve enhancing the cancer immunity cycle or reducing challenges to it. For example, chemotherapy, radiation, and oncolytic viruses can be used to initiate the cancer immunity cycle by killing off cancer cells, causing them to release antigens and danger signals that kickstart an immune response. Cancer vaccines or dendritic cells pre-loaded with antigens may also be used to deliver cancer antigens and activate the immune system. Of particular interest are cancer vaccines using neoantigens, which are based on specific mutations found in the cancer cells. Other therapies can be used to provide the extra “go” signals (such as cytokines) that activate T cells, or to block the natural checkpoints that would otherwise tell the T cells to slow down or stop. T cell therapy can also be used to deliver high numbers of T cells that recognize cancer antigens and are already activated and ready to attack. More therapies are also available to help T cells and other cancer-fighting immune cells to infiltrate tumors or take down the tumor’s defense systems so that infiltrating cells can remain strong in the intense fight against cancer cells.



