Oncolytic Viruses
What are oncolytic viruses?
To understand oncolytic viruses, it is first important to understand what viruses are.
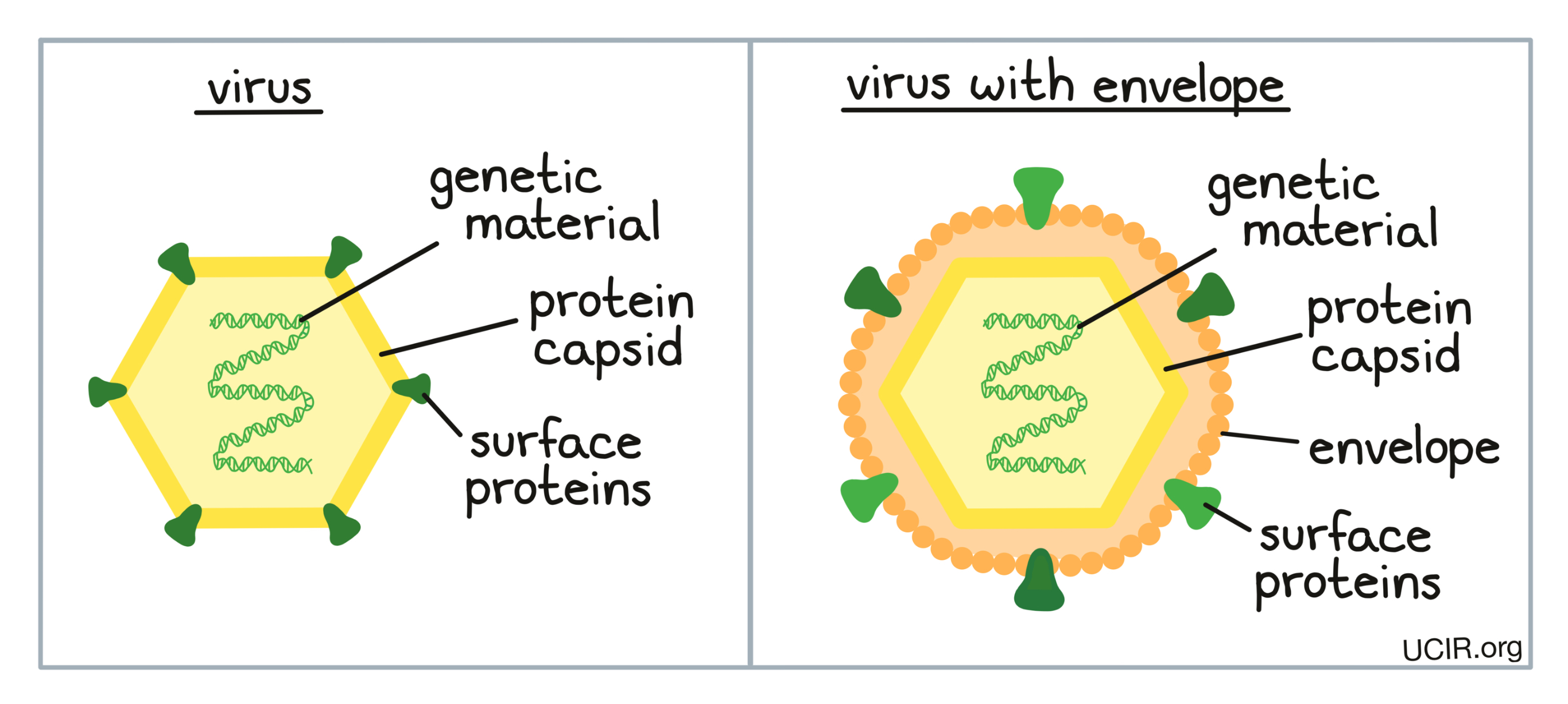
Viruses are tiny microorganisms which infect living creatures such as animals and people to reproduce and ultimately escape to infect others. Well-known viruses are the common cold virus, the flu virus, and HIV.
There are many different types and subtypes of viruses, however, they all share the same basic structure.Viruses carry a small amount of their own genetic material (DNA or RNA) enclosed in a sturdy shell called a capsid, which is sometimes surrounded by an outer membrane called the envelope. Surface proteins displayed on the membrane (or on the capsid if there is no membrane) are used by the virus to attach to the cells it is trying to infect.
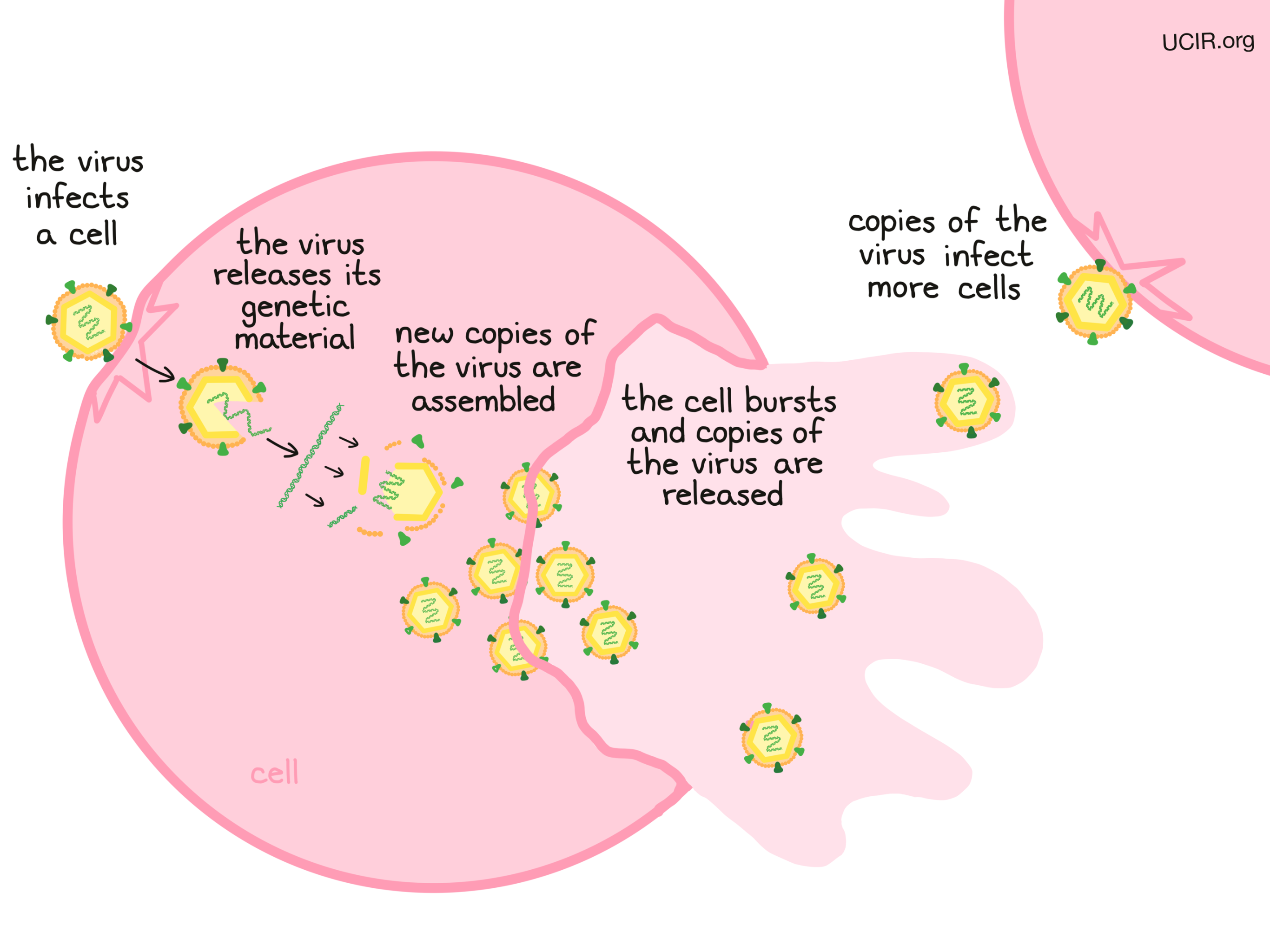
The details of how each virus reproduces is different, but in general, viruses reproduce by:
- Binding to a cell, entering the cell, and releasing genetic material
- Producing new viral proteins and copying the viral genes
- Assembling new copies of the virus from the viral proteins and the viral genes
- Exiting from the infected cell. This can occur slowly, by gradually releasing new virus through the cell membrane, or in a burst, as the cell explodes and releases many new copies of the virus at once. Usually, the cell producing the virus dies.
- The released virus goes on to infect new cells and the virus reproduction and cell killing continues.
Oncolytic viruses
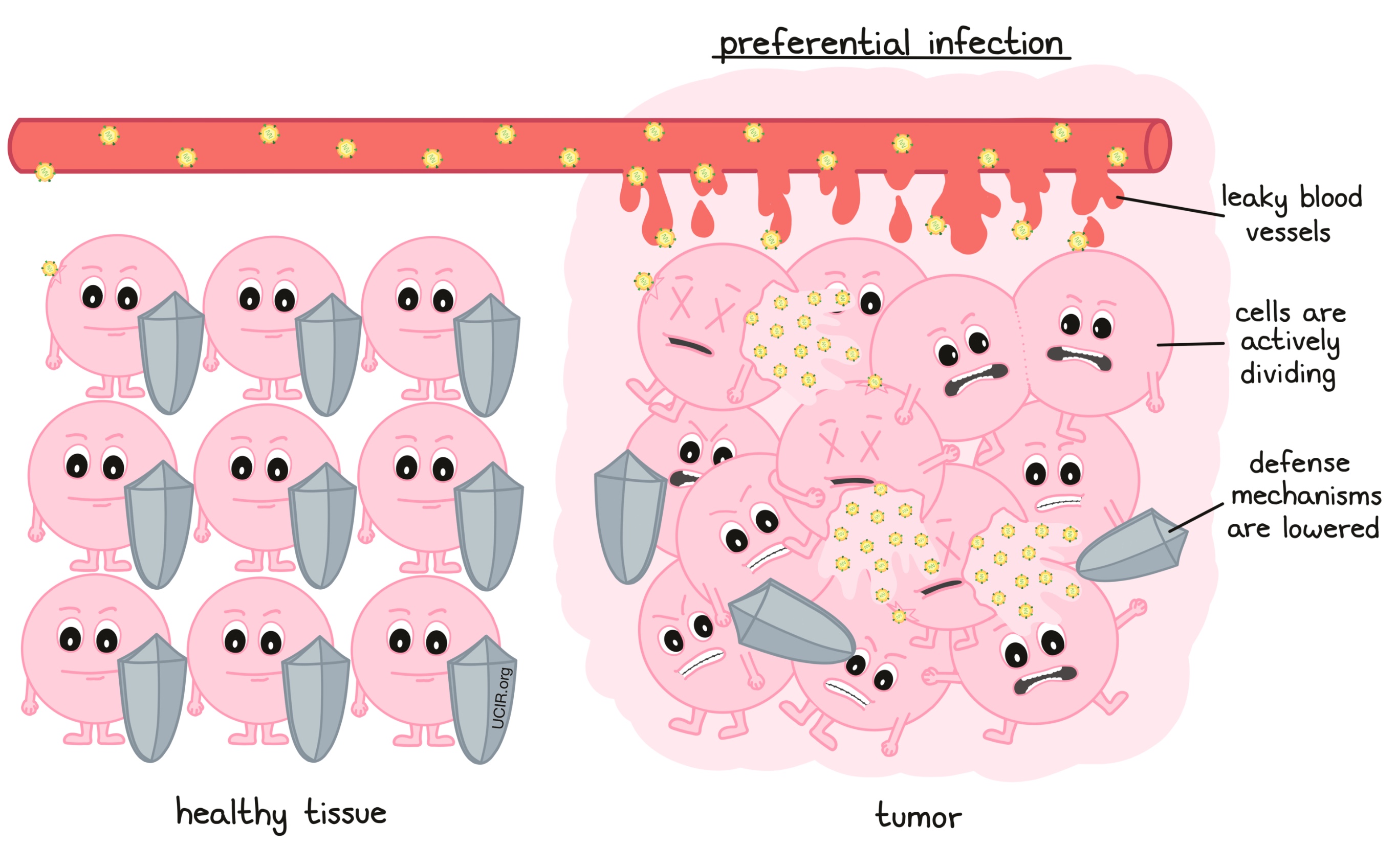
Oncolytic viruses preferentially infect and kill cancer cells while leaving healthy cells largely untouched. “Onco” is derived from “onkos”, meaning mass, in reference to tumor mass. “Lytic” is derived from “lysis”, which means to break into small pieces. Thus, oncolytic viruses are those that cause cancer cells to break apart and die as part of the virus’s reproduction process.
Certain cancer types are prone to infection with oncolytic viruses for a number of reasons. Some tumors are surrounded and infiltrated by leaky blood vessels, allowing the oncolytic viruses to enter the tumor tissue. Viruses also grow better in cells that are rapidly dividing, like cancer cells, rather than in normal cells, which divide less frequently. Many cancer cells also have defects in their defense mechanisms, leaving them more vulnerable to a viral attack.
How do oncolytic viruses trigger an immune response?
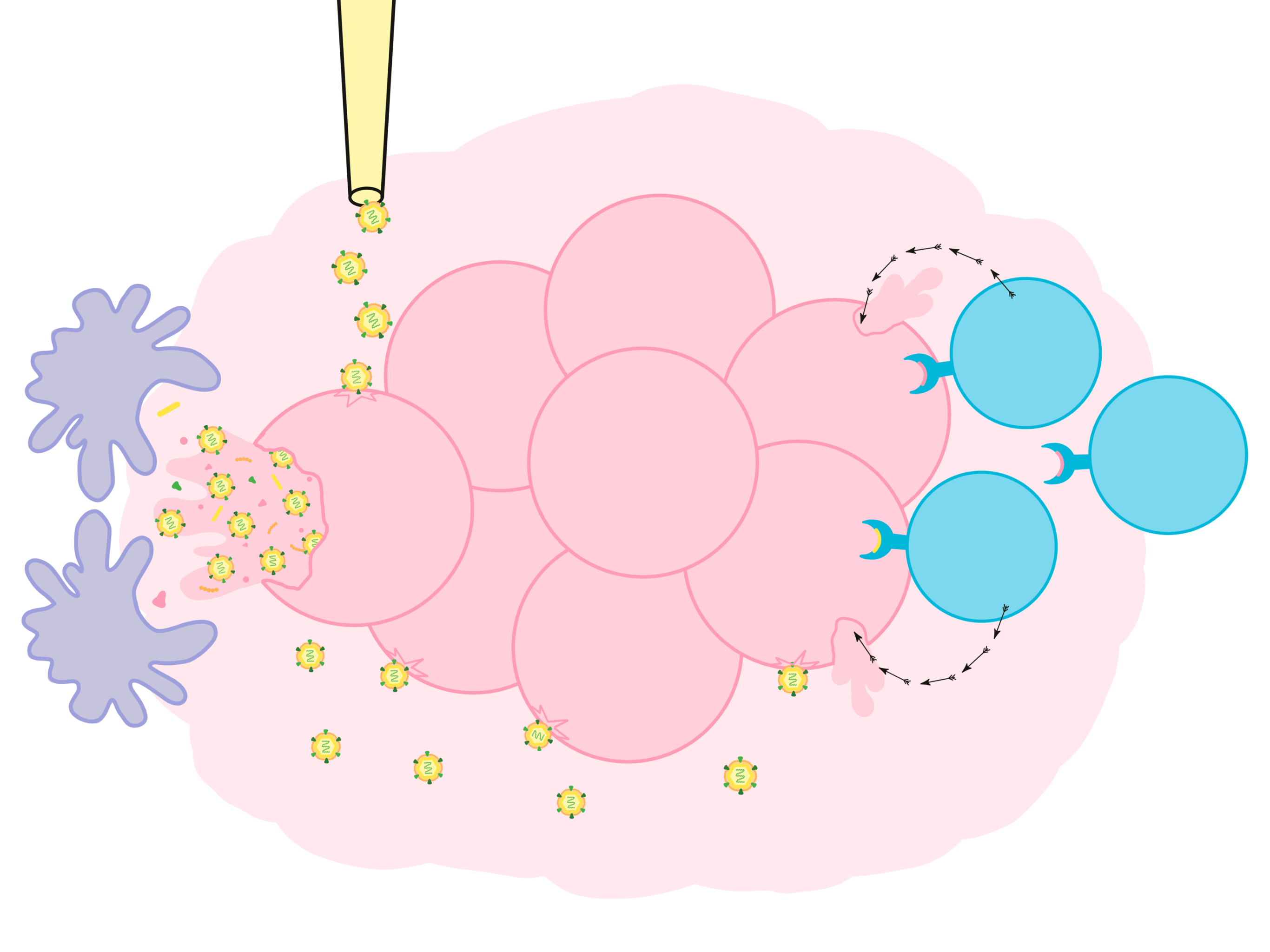
Oncolytic viruses offer multiple direct opportunities as cancer therapeutics. In addition to destroying cancer cells, oncolytic viruses also awaken an immune response against cancer cells, and this may be their most important anti-cancer activity. Oncolytic viruses stimulate the immune system in two different ways:
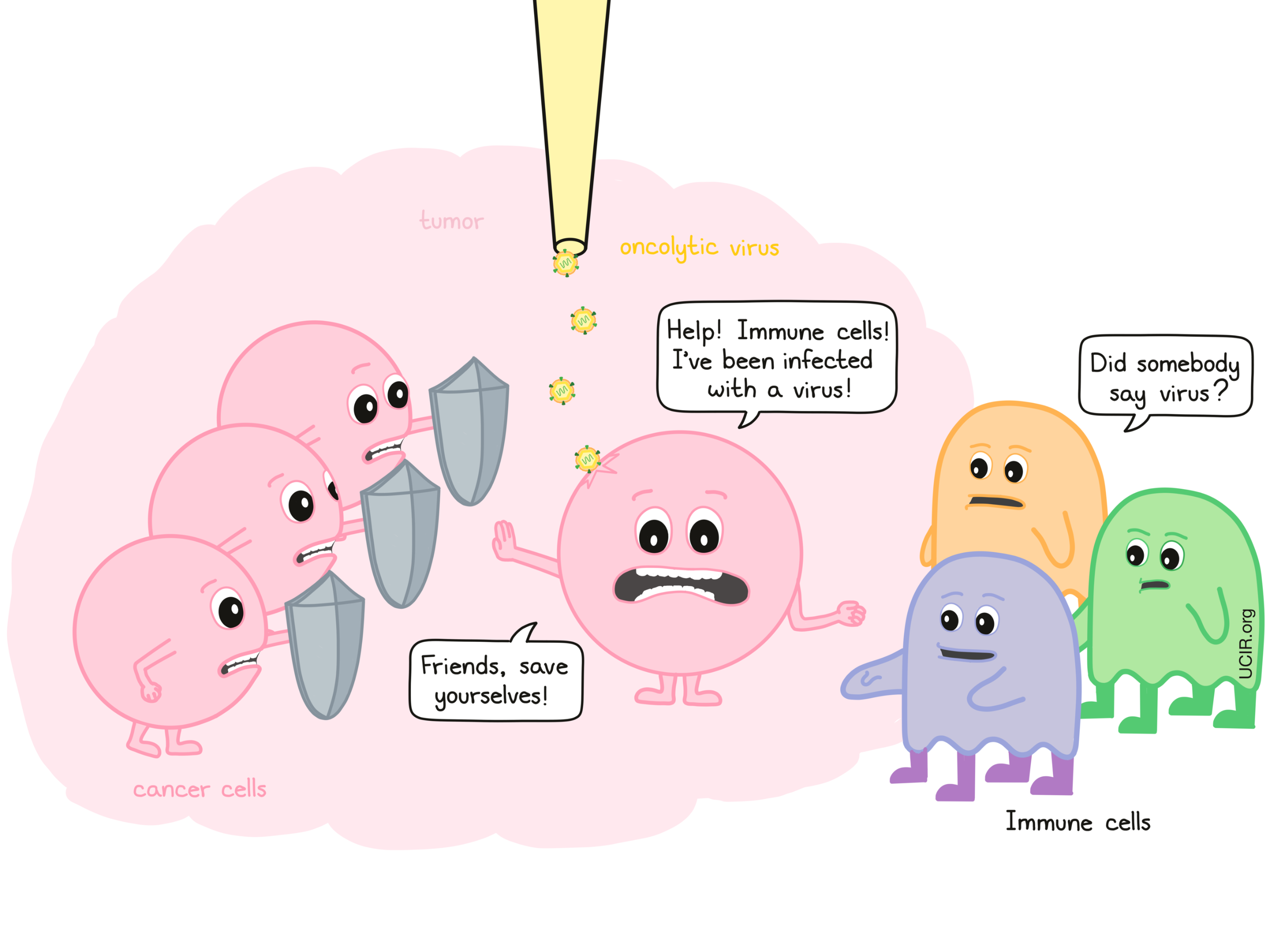
1. Virus-infected cells send signals that recruit immune cells to the tumor site
Viruses by themselves are recognized as a threat to the body. When a virus infects a cell, it triggers a cascading series of “antiviral” responses. The infected cell tries to limit viral reproduction within itself and also sends out molecules that act as warning signals, telling neighboring cells to activate their defense systems.
The molecules made by infected cells also alert the immune system and cause a local immune reaction by:
- recruiting immune cells to the area
- changing the local environment to make it easier for immune cells to migrate in; and
- activating immune cells to multiply and become more potent at killing infected cells.
These natural immune-stimulating properties of viruses are critical for the goal of developing a body-wide anti-cancer immune response.
2. Cancer cells killed by oncolytic viruses promote the development of immune cells that circulate throughout the body and kill cancer cells at other sites
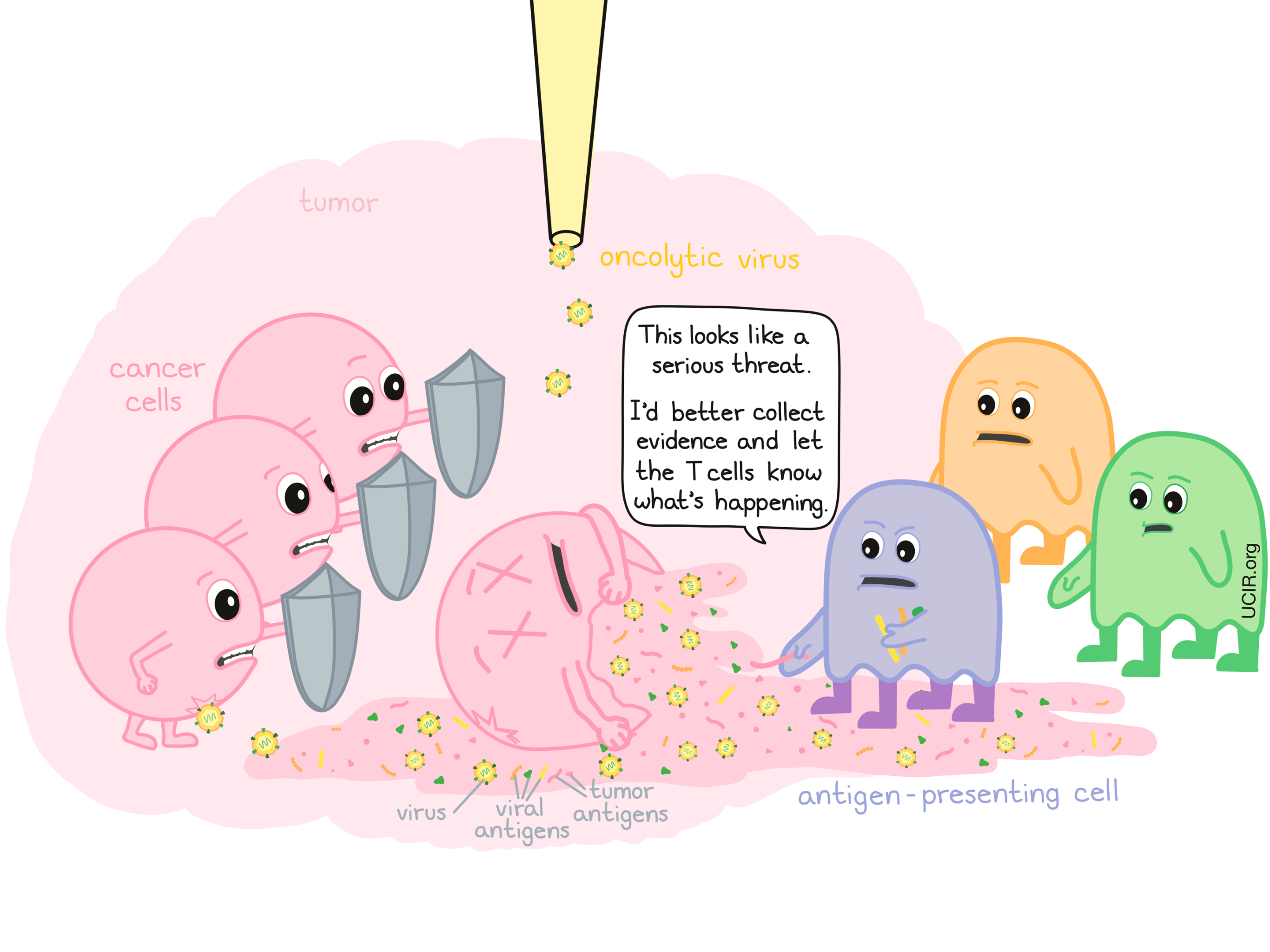
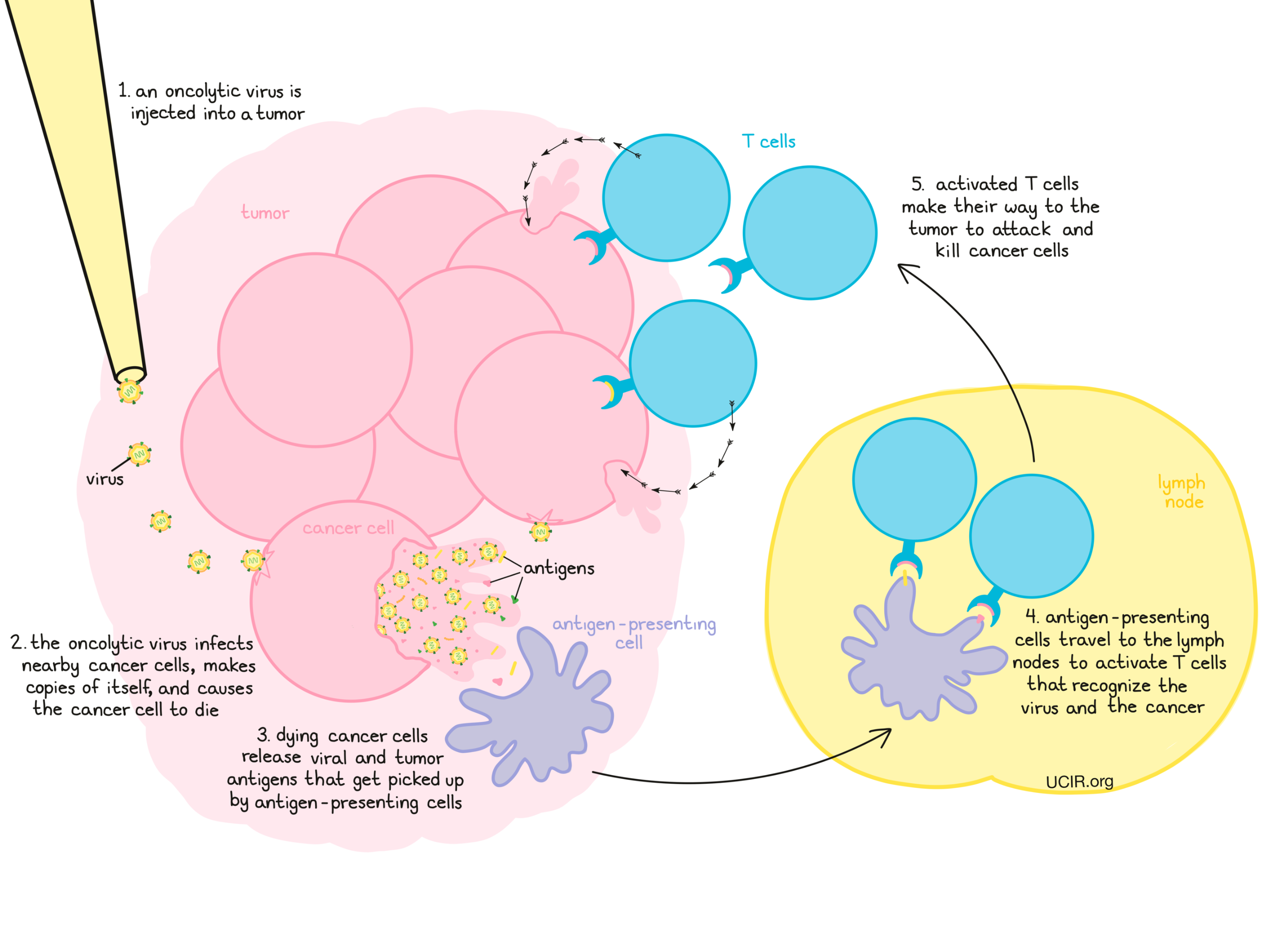
Immune cells called T cells can recognize and attack cells containing foreign molecules (like those from a virus) known as antigens. Similarly, cancer cells often make abnormal molecules, known as tumor antigens, although these often do not trigger a strong immune response.
When oncolytic viruses infect and destroy cancer cells, debris is released by the dying cells. This debris includes not only copies of the virus and viral antigens, but also cancer cell debris containing tumor antigens and molecules that alert the immune system of damage. These molecules attract the attention of antigen-presenting cells, which patrol the body and pick up antigens as evidence of a threat.
The antigen-presenting cells then travel to the lymph nodes and present this evidence to T cells; if the evidence is suspicious enough, then T cells become activated.
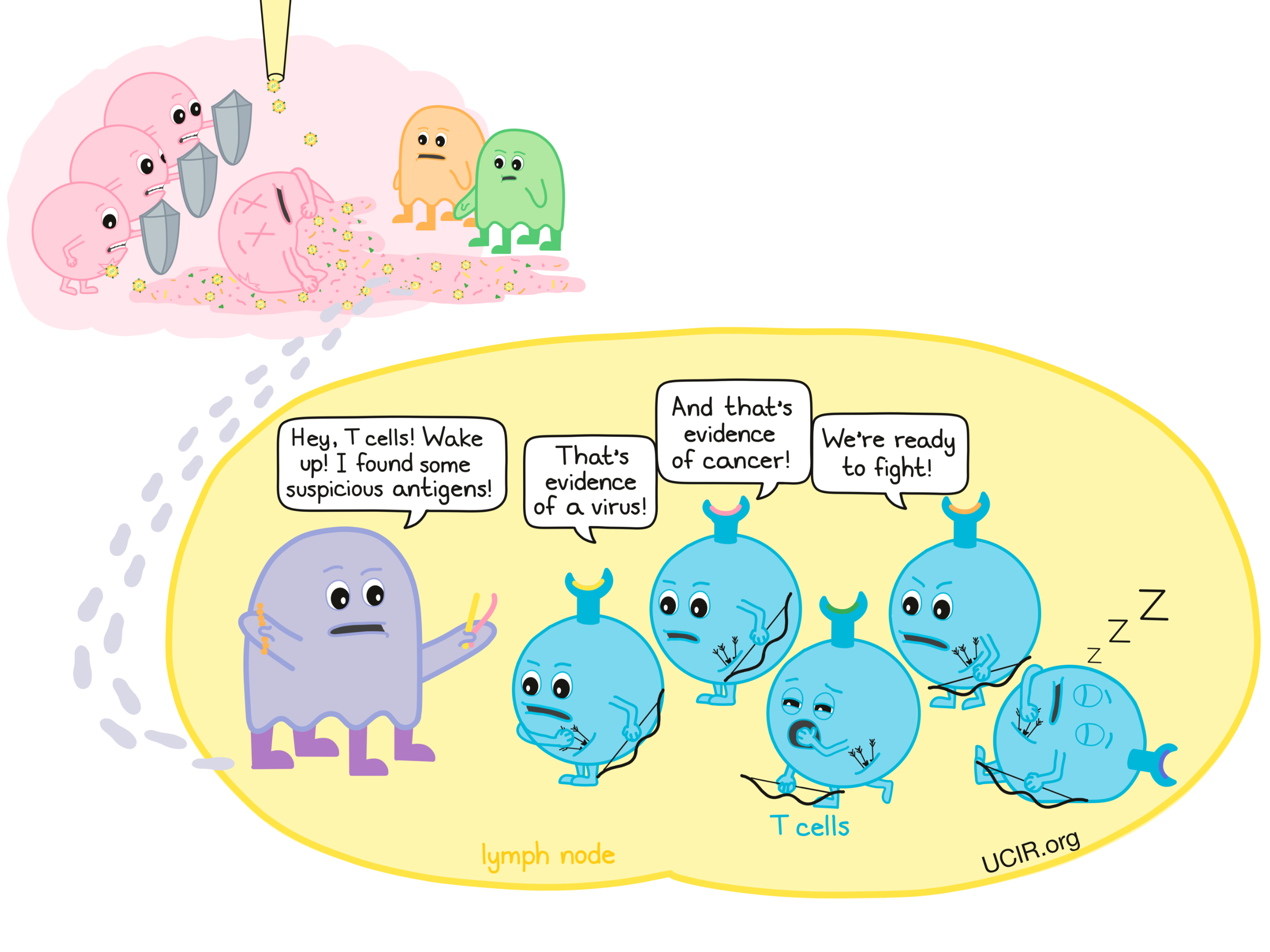
This initiates a two-pronged T cell response against tumors: T cells that were presented with viral antigens will go on to attack cancer cells because they are infected with the virus, and T cells that were presented with tumor antigens will go on to attack cancer cells because they are cancerous.
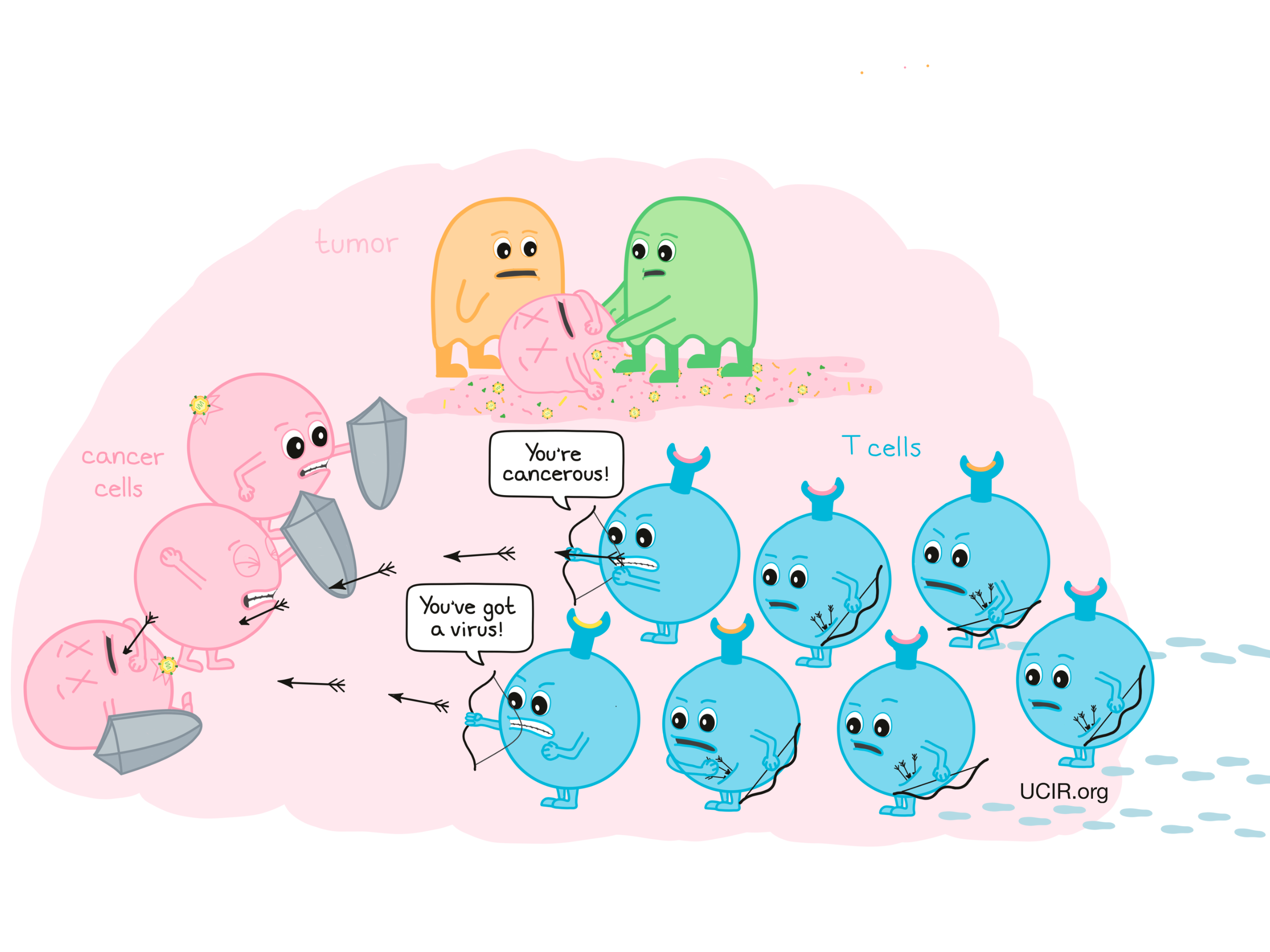
T cells can enhance the eradication of the tumor that was directly treated with the oncolytic virus, but can also circulate throughout the body and attack cancer cells that have spread to other sites. In addition, “memory” T cells are formed that can persist in the body for many years and are able to recognize and quickly restart an immune response to antigens they remember.
Oncolytic viruses in the clinic
In the more than a century since doctors noted that viral infections had anti-cancer effects in some patients, many viruses and treatment strategies were tested, but with only limited success.
A breakthrough came with the development of a carefully designed oncolytic virus, Imlygic (talimogene laherparepvec). Imlygic is based on herpes simplex virus type 1 (the virus that causes common cold sores), but the virus has been genetically engineered to improve its safety and immune-stimulating properties. The first clinical trials showed that when the virus was directly injected into tumors, it caused them to shrink. Importantly, injection of the oncolytic virus at one tumor site also caused tumors at distant, untreated sites to shrink. Further studies showed that the virus had stimulated an anti-cancer immune response.
Imlygic is approved for clinical use in melanoma and is now being tested in many other cancer types. Its success has re-energized efforts to explore and improve on the anti-cancer activity of other viruses. Many clinical trials that are recruiting patients can be found at clinicaltrials.gov.
Improving oncolytic viruses
Although some oncolytic viruses have shown very promising results in the clinic, research and development continues in multiple areas:
Administration of oncolytic viruses in the clinic
Viruses cannot spread throughout the body easily, so to increase the likelihood that the cancer cells get infected, oncolytic viruses are typically injected directly into tumor sites. Not all tumors are easily accessible though, and some guidance techniques are currently available, but more sophisticated techniques need to be developed to allow injection into difficult-to-reach tumors. In addition, existing viruses that can circulate in the blood and penetrate tissues are being developed as oncolytic viruses.
Antiviral immune response
Oncolytic viruses initiate immune responses against themselves, which can block the ability of the virus to spread. “Memory” T cell responses against the virus further affect how well subsequent treatment doses work. In addition, since many oncolytic viruses are derived from viruses common in the human population (e.g. herpes virus), some patients may have been exposed to the virus in the past and may already have protective immunity, even against the first dose. It may be possible to develop “stealth” viruses that do not generate immune responses against themselves that would hinder their ability to infect cancer cells.
Preferential infection and killing of cancer cells
While oncolytic viruses prefer to infect cancer cells, healthy cells may still get infected, or cancer cells may not be effectively infected or killed. Strategies to improve preferential infection and cancer cell killing include:
- identifying and engineering of oncolytic viruses that infect and kill additional cancer types;
- identifying viruses that bind to molecules that are abundantly present on cancer cells, but are rare on normal cells;
- changing genes within the virus so that binding of the virus to a molecule on the surface of cancer cells is enhanced; and
- changing genes within the virus so that the virus can only multiply in cancer cells and eventually kill them.
Immune-stimulating activity
Strategies to improve the immune-stimulating activity of oncolytic viruses include:
- adding genes to the virus to help stimulate an immune response to the cancer cells;
- removing viral genes that suppress immune responses; and
- adding known tumor antigens to the virus to help focus the anti-cancer immune response.
Combination of oncolytic viruses with standard cancer therapies and/or other immunotherapies
The significant anti-cancer effect seen with Imlygic in causing tumors to shrink not only at injected tumor sites, but also at distant sites, proves the immune-stimulating activity of the viral infection. Combining oncolytic viruses with conventional cancer therapeutics that have immune-stimulating properties (e.g. chemotherapy, radiation) or with modern immunotherapies (e.g. checkpoint blockade)is a logical strategy to further enhance the antitumor immune responses that are initiated by oncolytic viruses.
Further information
Scientific references:
- Oncolytic Viruses in Cancer Treatment: A Review Lawler SE, Speranza MC, Cho CF, Chiocca EA. JAMA Oncology (2017)
- The Current Status and Future Prospects of Oncolytic Viruses in Clinical Trials against Melanoma, Glioma, Pancreatic, and Breast Cancers Eissaet al. Cancers (Basel) (2018)
- Talimogene laherparepvec: review of its mechanism of action and clinical efficacy and safety Raman SS, Hecht JR, Chan E. Immunotherapy (2019)


