Approval in the US
The US product name for Blitzima is Rituxan.
How is the drug name pronounced?
Rituximab: Ri-TUX-i-mab
Blitzima: Blit-ZEEM-ah
Blitzima (rituximab) is “biosimilar” to MabThera (rituximab). Blitzima has been shown to be similar to MabThera in the way in which it works, how well it works, and how safe it is. Other approved drugs that are biosimilar to MabThera are Truxima, Ritemvia, Riximyo, and Rixathon.
The US product name for MabThera is Rituxan.
What cancer(s) does this drug treat?
Blitzima targets the CD20 molecule found on most B cells, and is only indicated for cancers that test positive for CD20.
B-cell Non-Hodgkin lymphoma (NHL)
Blitzima is approved for:
- Adult patients with stage 3-4 follicular B-cell Non-Hodgkin lymphoma whose cancer did not respond to previous treatment with chemotherapy, or responded to two or more previous chemotherapy treatments but has since returned.
- Adult patients with previously untreated stage 3-4 follicular B-cell Non-Hodgkin lymphoma. In such cases, Blitzima is given in combination with chemotherapy.
- Adult patients with follicular B-cell Non-Hodgkin lymphoma who have been successfully treated. In such cases, Blitzima is given as maintenance therapy to prevent the cancer from getting worse or coming back.
- Adult patients with diffuse large B-cell lymphoma (DLBCL). In such cases, Blitzima is given in combination with cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) chemotherapy.
- Pediatric patients (6 months to 18 years old) with previously untreated advanced stage diffuse large B-cell lymphoma (DLBCL), Burkitt lymphoma (BL)/Burkitt leukemia (mature B-cell acute leukemia) (BAL) or Burkitt-like lymphoma (BLL) in combination with chemotherapy.
Chronic lymphocytic leukemia (CLL)
Blitzima is approved for:
- Adult patients with chronic lymphocytic leukemia who have previously been untreated or treated, but the cancer either did not respond to treatment or has since returned. In such cases, Blitzima is given in combination with chemotherapy.
Limitations of Use
Age: The safety and efficacy of Blitzima have not been established in patients under 18 years of age in any cancer indication other than previously untreated advanced stage diffuse large B-cell lymphoma (DLBCL), Burkitt lymphoma (BL)/Burkitt leukemia (mature B-cell acute leukemia) (BAL) or Burkitt-like lymphoma (BLL). Blitzima should not be used in patients younger than 6 months of age.
Infections: Blitzima can weaken the immune system and is not recommended for use in patients who currently have or recently had a severe infection. Patients will be screened for the hepatitis B virus prior to Blitzima treatment. In patients who had hepatitis B in the past, or who are carriers of the hepatitis B virus, Blitzima can cause the virus to become active again. These patients will need to be monitored closely during treatment and for several months after Blitzima treatment. Patients with active hepatitis B disease should not be treated with Blitzima.
Exclusions: Patients with a weakened or impaired immune system should not be treated with Blitzima.
Vaccinations: Live virus vaccinations (e.g. chickenpox or measles, mumps, and rubella (MMR)) less than 4 weeks prior to or during Blitzima treatment are not recommended.
Pregnancy/breastfeeding: Blitzima can cause harm to a fetus and is not recommended for use during pregnancy. Women who are able to become pregnant should use effective birth control while receiving Blitzima, and for twelve months after the last dose of Blitzima. Due to the potential for serious adverse reactions in a breastfed child, women are also advised not to breastfeed during treatment and for at least six months after the last dose of Blitzima.
What type of immunotherapy is this?
- Cell-killing antibody
How does this drug work?
Target:
- CD20 molecule on B cells
Blitzima is an antibody that was made in the laboratory. Blitzima and other antibody molecules have an overall “Y” shape. The two tips of the upper arms of the “Y” shape are the parts of the antibody that can very precisely bind to its target. Blitzima binds to a molecule called CD20 on the surface of a cancerous B cell. CD20 is commonly found on the surface of cancer cells in patients with Non-Hodgkin lymphoma and chronic lymphocytic leukemia (CLL). CD20 can also be found on the surface of all normal human B cells, which means that in addition to attacking cancer cells, Blitzima can also attack healthy B cells.
The stem of Blitzima’s “Y” shape has binding sites for immune cells or other parts of the immune system.
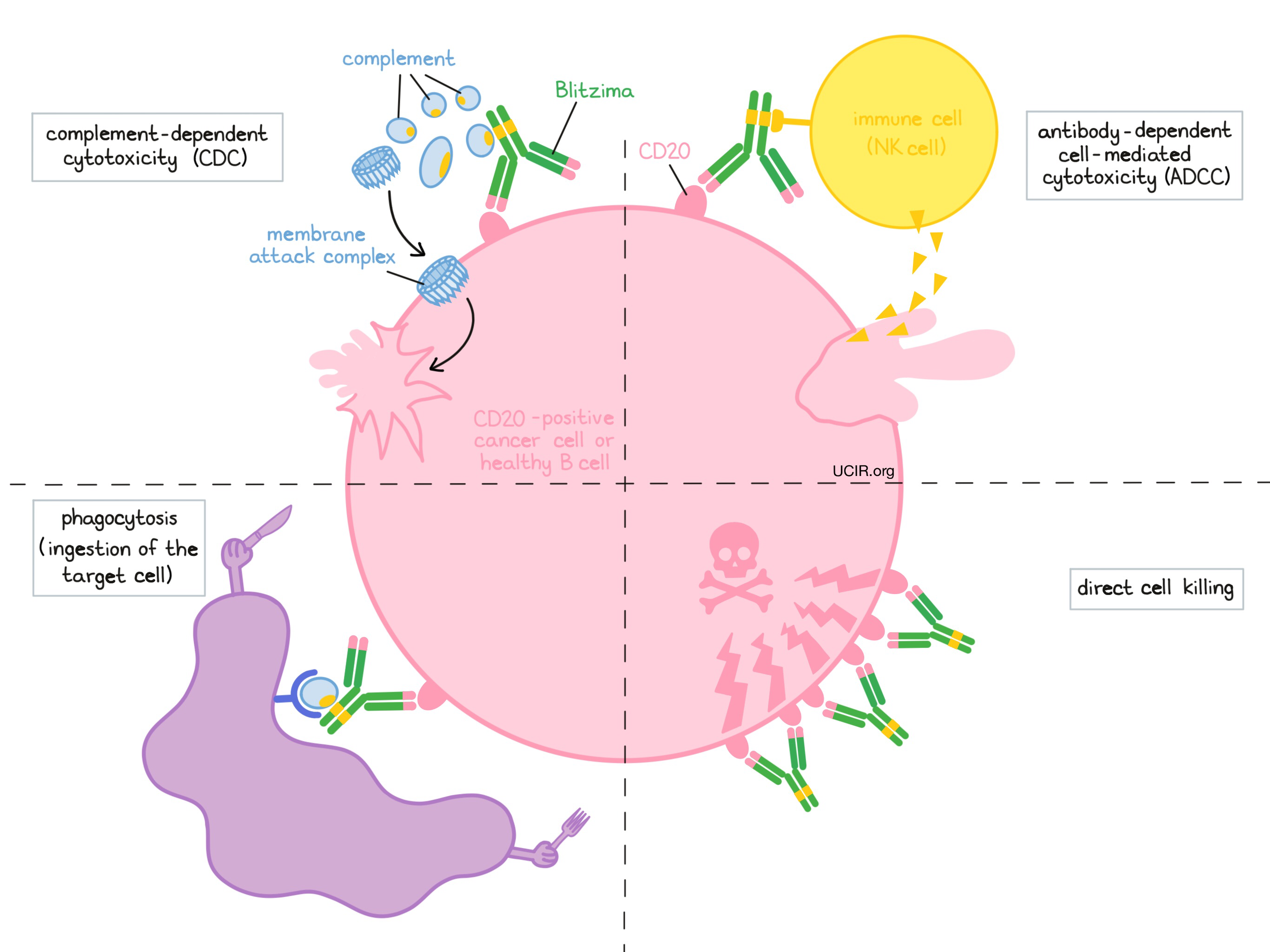
At least four different mechanisms are thought to be responsible for the elimination of CD20-positive B cells by Blitzima. Blitzima is helped by the immune system to kill cancer cells and may also work alone.
Complement-dependent cytotoxicity (CDC)
When bound to CD20 on the surface of cancerous or normal B cells, the “stem” of Blitzima can attract and bind molecules of the immune system that freely flow in the blood or tissues, and are called “complement”. Activation of the complement system causes the formation of the “membrane attack complex”, which can puncture and destroy the cell that Blitzima is bound to. This is understood to be the main way through which Blitzima kills cells.
Antibody-dependent cell-mediated cytotoxicity (ADCC)
When bound to CD20 on the surface of cancerous or normal B cells, the “stem” of Blitzima can also attract and bind immune cells (like NK cells). This allows Blitzima to act as a bridge between the target cell and the immune cell. The immune cell then releases molecules that can kill the cell Blitzima is bound to.
Phagocytosis
When Blitzima is bound to cancerous or normal B cells, it can also attract immune cells, called phagocytes, that have the ability to ingest (“eat”) cells that have been coated with Blitzima or parts of the complement system. Phagocytosis is not a major way through which Blitzima kills cells.
Direct cell killing
By binding to CD20 molecules on the surface of cancerous or normal B cells and bringing the CD20 molecules close together in “clusters”, Blitzima can directly cause the cells to die, although this is not a major way through which Blitzima kills cells.
The combined effect of these mechanisms results in the elimination of cancerous and normal B cells from the body. A new population of healthy B cells can then develop from blood-forming ‘stem’ cells that reside in the bone marrow.
How is this drug given to the patient?
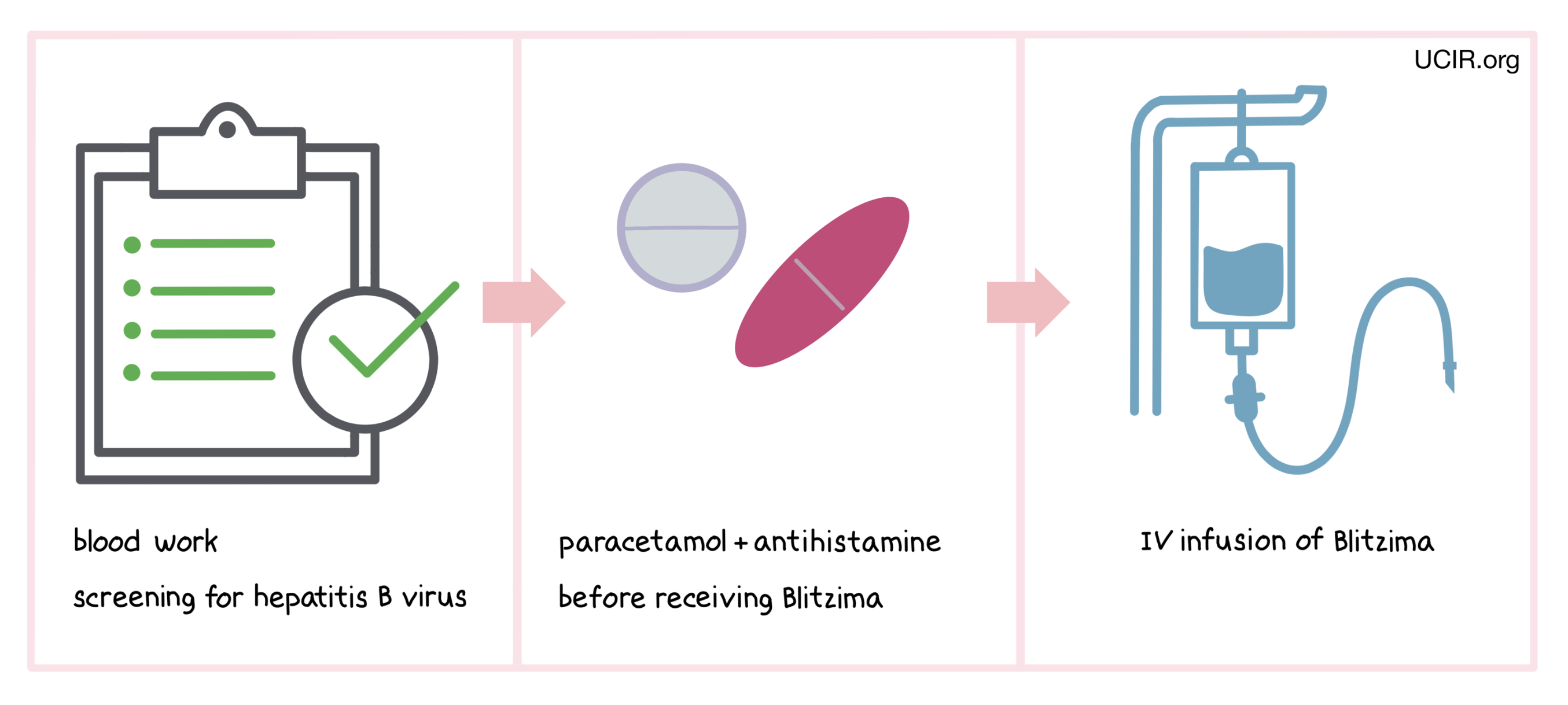
Blitzima is administered through a tube in the vein (intravenous infusion, or i.v.) every week for 4-8 doses when given alone. The treatment schedules for Blitzima as maintenance therapy or in combination with chemotherapy may be different. Patients will receive paracetamol and an antihistamine prior to each infusion in order to reduce the risk of infusion-related side effects. In some cases patients may also receive glucocorticoids before Blitzima treatment. Administration of Blitzima does not require a hospital stay.
Before starting Blitzima therapy, patients will need to get blood tests done to check if the patient is a carrier of the hepatitis B virus. Blitzima can cause the virus to become active again, and the patients who test positive for the hepatitis B virus will need to be monitored more closely during treatment and for several months afterward. Blood tests are also used to obtain complete blood counts prior to each course of Blitzima and on a regular basis during treatment, if needed. This is because reductions in the number of blood cells are particularly common in patients being treated with Blitzima.
Patients with chronic lymphocytic leukemia (CLL) will also receive treatment (adequate hydration and uricostatics) before infusion with Blitzima to reduce the risk of tumor lysis syndrome (inflammation due to rapid breakdown of the tumor) and decrease the risk and severity of reactions to the infusion.
The first infusion of Blitzima is administered more slowly than subsequent infusions (over 4 to 6 hours) in order to monitor for infusion-related reactions. Such reactions are very common side effects of Blitzima treatment and usually occur within 24 hours after the infusion. If symptoms of an infusion-related reaction occur at any point during the first infusion or any subsequent infusions, the infusion may be interrupted or slowed, depending on the severity of the reaction. It is important that patients discuss with their doctor if they notice any changes following a Blitzima infusion, as infusion-related reactions are very serious and can be fatal.
What are the observed clinical results?
For:
Follicular B-cell Non-Hodgkin lymphoma (previously treated)
Follicular B-cell Non-Hodgkin lymphoma (previously untreated)
Follicular B-cell Non-Hodgkin lymphoma (previously successfully treated with chemotherapy and a rituximab product)
Diffuse large B-cell lymphoma (DLBCL; previously untreated)
Mature B-cell Non-Hodgkin lymphoma in children
Chronic lymphocytic leukemia (CLL)
It is important to keep in mind that each patient’s actual outcome is individual and may be different from the results found in the clinical studies. In addition, immunotherapy can sometimes take several months to yield an observable treatment response.
Follicular B-cell Non-Hodgkin lymphoma (previously treated)
In a clinical trial of 166 patients with low-grade or follicular B-cell Non-Hodgkin lymphoma who had been previously treated, but the cancer either did not respond to treatment or had since returned, patients were treated with rituximab (rituximab is the active ingredient in Blitzima). Overall, 48% of the patients responded to treatment (tumors shrank or went away completely), including 6% of participants whose tumor went away completely. Patients did not experience a worsening or return of their disease for a median of 13 months.
In another clinical trial of 58 patients with low-grade or follicular B-cell Non-Hodgkin lymphoma who had previously responded to a rituximab product (MabThera or one of its equivalents, e.g. Blitzima), but the cancer had since returned, patients were re-treated with rituximab. 38% of the patients responded to retreatment with rituximab, including 10% whose tumor went away completely. Patients did not experience a worsening or return of their disease for a median of 18 months, compared to 12 months for the prior treatment with a rituximab product.
In the two trials above, 39 patients had bulky disease (a single tumor with more than 10 cm in diameter). 36% of these participants responded to retreatment with rituximab, including 3% whose tumors went away completely. Patients did not experience a worsening or return of their disease for a median of 10 months.
Follicular B-cell Non-Hodgkin lymphoma (previously untreated)
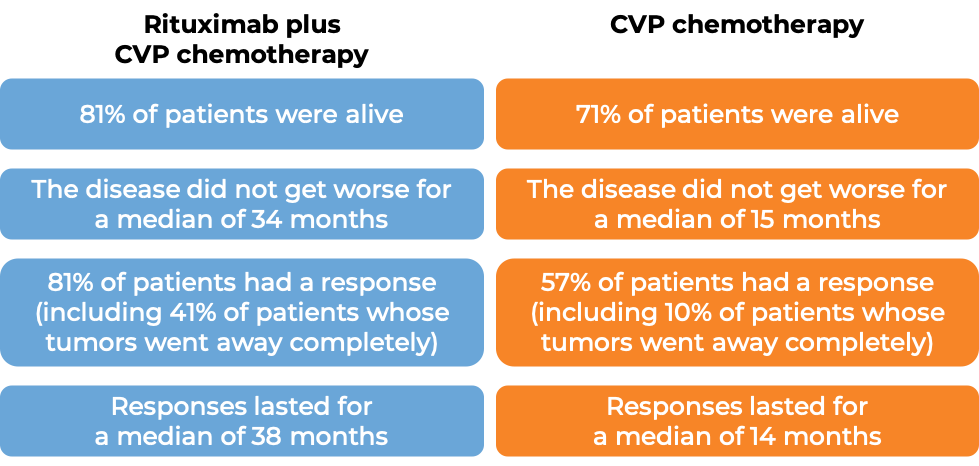
In a clinical trial of 321 patients with previously untreated follicular B-cell Non-Hodgkin lymphoma, patients were treated with either rituximab (rituximab is the active ingredient in Blitzima) plus cyclophosphamide, vincristine, and prednisone (CVP) chemotherapy, or with CVP chemotherapy alone. At a median follow-up of 53 months:
Results from three other clinical trials using rituximab (rituximab is the active ingredient in Blitzima) in combination with chemotherapy other than CVP, including:
- cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) chemotherapy, OR
- mitoxantrone, chlorambucil, and prednisone (MCP) chemotherapy, OR
- cyclophosphamide, doxorubicin, teniposide, and prednisone (CHVP) chemotherapy plus interferon-α
have demonstrated similar clinical improvements for patients compared to the corresponding chemotherapy treatment alone.
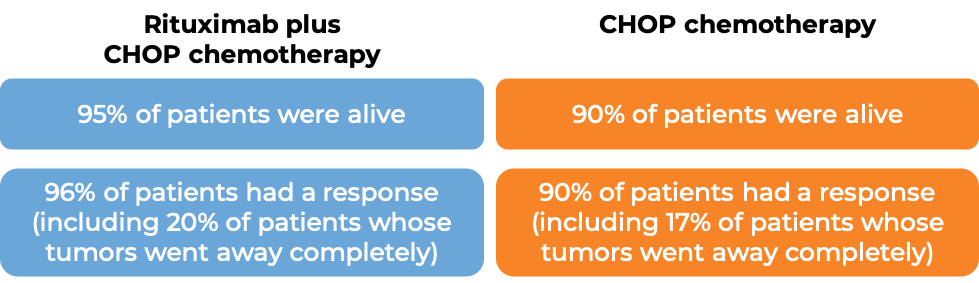
428 patients with previously untreated follicular B-cell Non-Hodgkin lymphoma were treated with either rituximab (rituximab is the active ingredient in Blitzima) plus cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) chemotherapy, or with CHOP chemotherapy alone. At a median follow-up of 18 months:
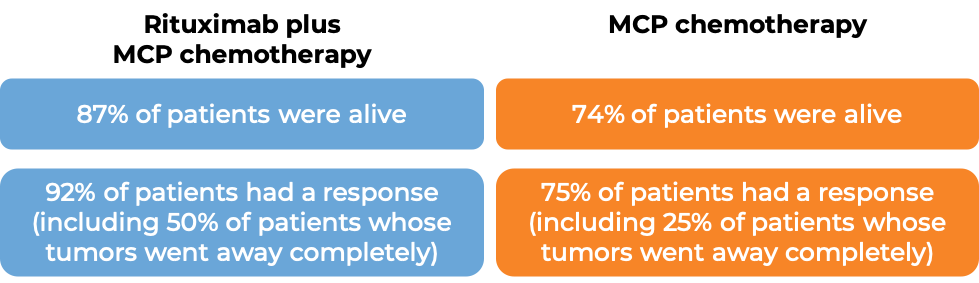
201 patients with previously untreated follicular B-cell Non-Hodgkin lymphoma were treated with either rituximab (rituximab is the active ingredient in Blitzima) plus mitoxantrone, chlorambucil, and prednisone (MCP) chemotherapy, or with MCP chemotherapy alone. At a median follow-up of 4 years:
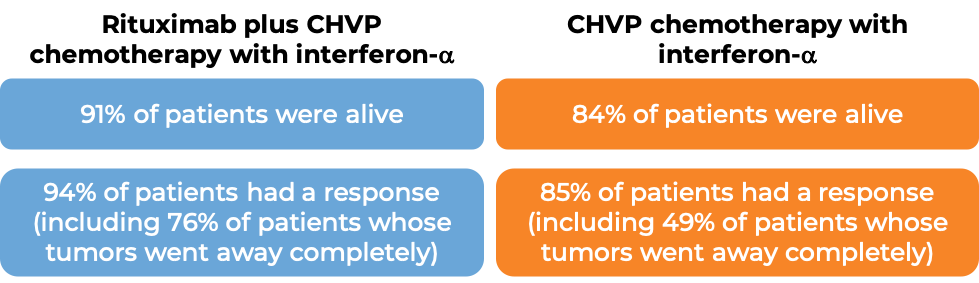
358 patients with previously untreated follicular B-cell Non-Hodgkin lymphoma were treated with either rituximab (rituximab is the active ingredient in Blitzima) plus cyclophosphamide, doxorubicin, teniposide, and prednisone (CHVP) chemotherapy with interferon-α, or with CHVP-interferon-α therapy alone. At a median follow-up of 42 months:
Follicular B-cell Non Hodgkin lymphoma (previously successfully treated with chemotherapy and a rituximab product)
In a clinical trial of 1193 patients with previously untreated advanced follicular B-cell Non-Hodgkin lymphoma, patients were treated with a rituximab product (MabThera or one of its equivalents, e.g. Blitzima) plus chemotherapy according to the investigators’ choice, including:
- cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) chemotherapy, OR
- cyclophosphamide, vincristine, and prednisone (CVP) chemotherapy, OR
- fludarabine, cyclophosphamide, and mitoxantrone (FCM) chemotherapy
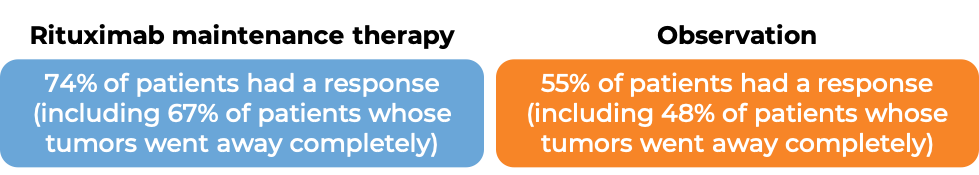
A total of 1078 patients responded to this first therapy, of which 1018 were either treated with rituximab as maintenance therapy to prevent the cancer from getting worse or coming back, or were left untreated. At a median follow-up of 25 months:
The long-term benefit of rituximab maintenance therapy was evaluated at a median follow-up of 9 years for all patients on the trial:
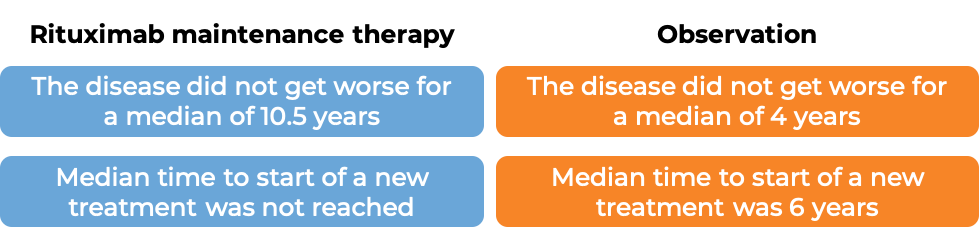
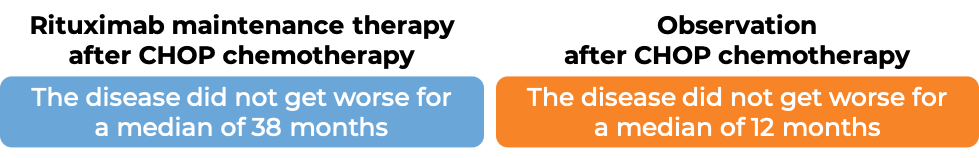
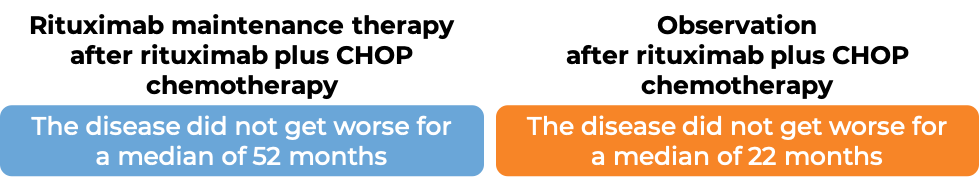
In another clinical trial of 465 patients with previously treated follicular B-cell Non-Hodgkin lymphoma, patients were treated with either rituximab (rituximab is the active ingredient in Blitzima) plus cyclophosphamide, doxorubicin, vincristine, and prednisolone (CHOP) chemotherapy or CHOP chemotherapy alone. A total of 334 patients saw their tumors shrink or disappear in response to this treatment, and those 334 patients were either treated with rituximab as maintenance therapy to prevent the cancer from getting worse or coming back, or were left untreated. At a median follow-up of 28 months for all patients on the trial after starting maintenance therapy or observation:
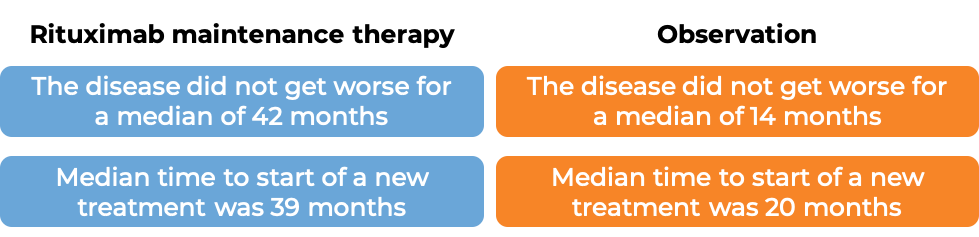
The benefit of rituximab maintenance treatment compared to observation was confirmed in all subgroups analysed, regardless of initial treatment (rituximab product plus CHOP chemotherapy or CHOP chemotherapy alone) or the quality of response to initial treatment (tumor shrinkage or complete tumor disappearance). However, patients who were treated with a rituximab product plus CHOP chemotherapy before starting rituximab maintenance therapy showed better disease control during the maintenance phase than patients treated with CHOP chemotherapy alone.
Diffuse large B-cell lymphoma (DLBCL; previously untreated)
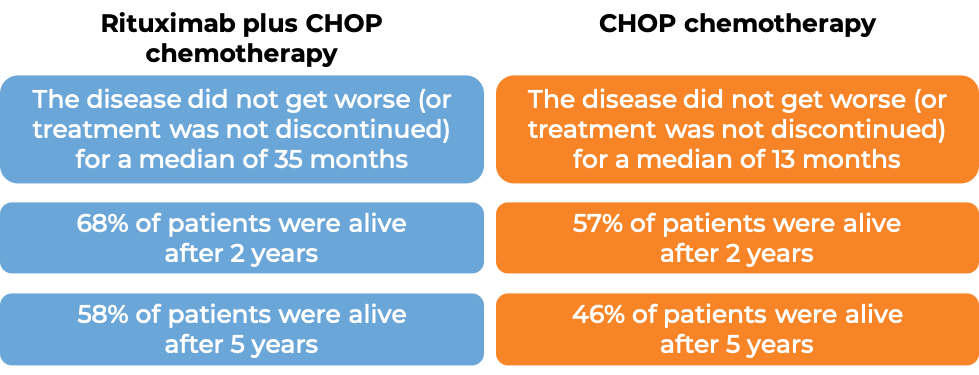
In a clinical trial of 399 patients aged 60 to 80 with previously untreated diffuse large B-cell lymphoma (DLBCL), patients were treated with either rituximab (rituximab is the active ingredient in Blitzima) plus cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) chemotherapy, or with CHOP chemotherapy alone. At a median follow-up of 31 months for all patients on the trial:
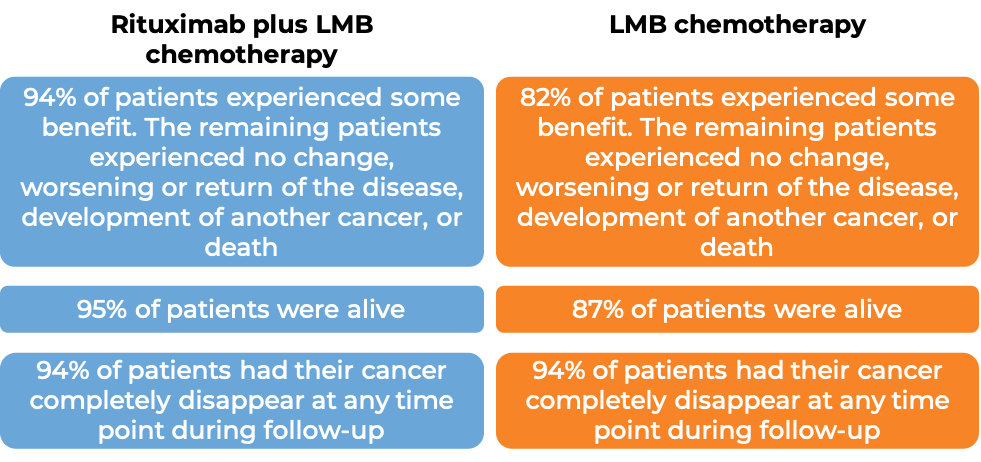
Mature b-cell Non-Hodgkin lymphoma in children
In a clinical trial of 328 pediatric patients, aged 6 months to 18 years, with previously untreated advanced diffuse large B-cell lymphoma (DLBCL), Burkitt lymphoma (BL)/Burkitt leukaemia (mature B-cell acute leukaemia) (BAL) or Burkitt-like lymphoma (BLL), patients were treated with either
- rituximab (rituximab is the active ingredient in Blitzima) plus Lymphome Malin B (LMB) chemotherapy OR
- Lymphome Malin B (LMB) chemotherapy alone (LMB chemotherapy: corticosteroids, vincristine, cyclophosphamide, high-dose methotrexate, cytarabine, doxorubicin, etoposide, and triple drug [methotrexate/cytarabine/corticosteroid] therapy, which is injected into the fluid-filled space between the thin layers of tissue that cover the spinal cord)
At a median follow-up of 3 years:
Chronic lymphocytic leukemia (CLL)
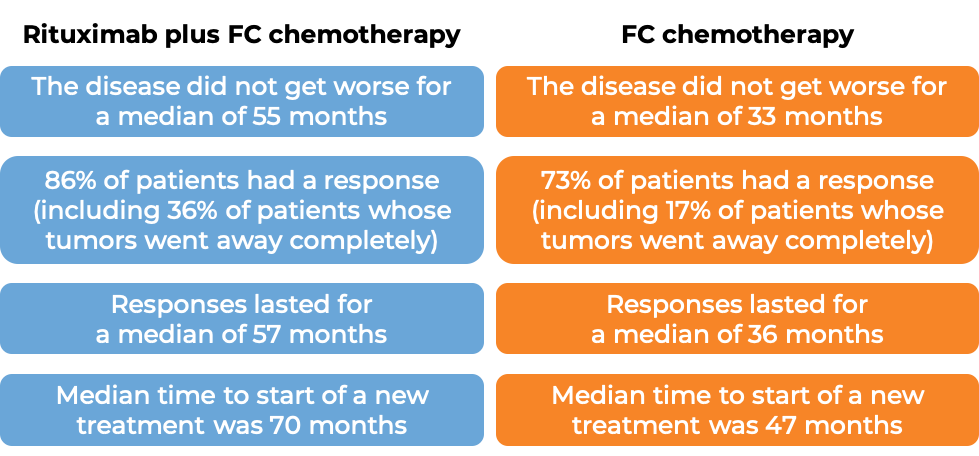
Previously untreated CLL
In a clinical trial of 817 patients with previously untreated chronic lymphocytic leukemia, patients were treated with either rituximab (rituximab is the active ingredient in Blitzima) plus fludarabine and cyclophosphamide (FC) chemotherapy, or with FC chemotherapy alone. At a median follow-up of 4 years for all patients on the trial:
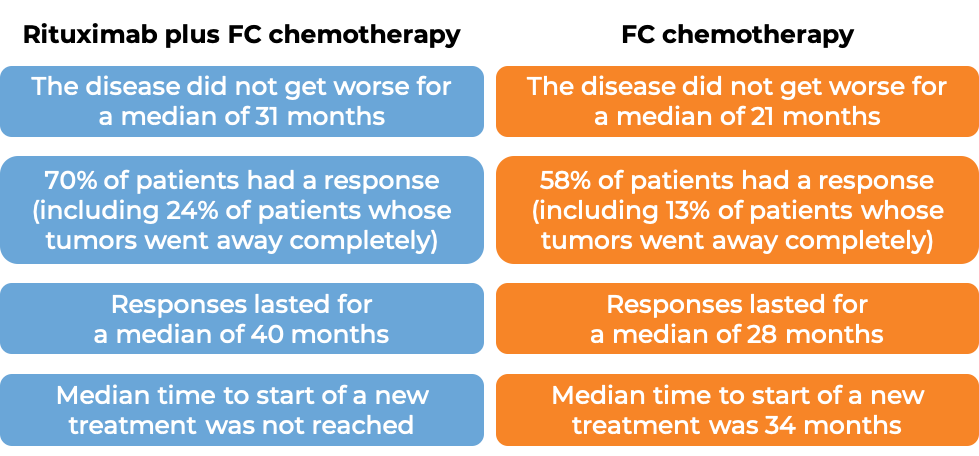
Previously treated CLL
In a clinical trial of 522 patients with previously treated chronic lymphocytic leukemia, patients were treated with either rituximab (rituximab is the active ingredient in Blitzima) plus fludarabine and cyclophosphamide (FC) chemotherapy, or with FC chemotherapy alone. At a median follow-up of 2 years for all patients on the trial:
Results from other clinical studies using rituximab (rituximab is the active ingredient in Blitzima) in combination with chemotherapy other than FC, including:
- cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) chemotherapy, OR
- fludarabine, cyclophosphamide, and mitoxantrone (FCM) chemotherapy, OR
- paclitaxel and carboplatin (PC) chemotherapy, OR
- paclitaxel, cyclophosphamide, and mitoxantrone (PCM) chemotherapy, OR
- bendamustine and cladribine chemotherapy
have shown clinical benefit for patients with previously treated or untreated CLL compared to the corresponding chemotherapy treatment alone.
Data from approximately 180 patients who had been previously treated with a rituximab product (MabThera or one of its equivalents, e.g. Blitzima) and were then again treated with a rituximab product have shown clinical benefit.
What are the potential side effects?
Blitzima targets the CD20 molecule, which, while present on cancerous B cells, is also present on normal B cells. As a result, Blitzima can kill normal B cells, increasing the risk of serious infections. Other common side effects of Blitzima include low white blood cell count and low red blood cell count.
Some side effects, such as reactions related to the infusion, severe skin and mouth reactions, severe infections, infections of the brain, hepatitis B virus reactivation, tumor lysis syndrome, heart problems, kidney problems, and stomach or bowel problems such as blockage or tears in the bowel, may be severe or life-threatening. Patients and caregivers receive careful instructions to monitor for signs and symptoms of these complications, and a healthcare provider should be immediately notified if symptoms occur. These conditions are managed by the health care provider.
Infusion-related reactions
Reactions to the Blitzima infusion are common and usually occur within 24 hours after the infusion. Some of these reactions are serious and can be fatal. Symptoms include hives, rashes, swelling of lips, tongue, or face, sudden cough, shortness of breath, difficulty breathing, dizziness or feeling faint, heart racing or fluttering, and chest pain. Reactions to Blitzima infusion may be caused by a combination of a widespread release of molecules called cytokines or other inflammatory substances, tumor lysis syndrome (inflammation due to rapid breakdown of the tumor), and severe allergic or hypersensitivity reactions.
Severe skin and mouth reactions
Severe skin and mouth reactions can include blisters, peeling skin, rashes, and painful sores or ulcers on the skin, lips, or in the mouth.
Serious infections and hepatitis B virus reactivation
Blitzima can reduce the immune system’s ability to fight off bacterial, fungal, and viral infections, can increase a patient’s risk of getting an infection, and can cause the reactivation of prior virus infections. These infections can be serious, and may be fatal. Symptoms of infection include: fever; cold symptoms, such as a persistently runny nose or sore throat; flu symptoms, such as coughing, tiredness, and achiness; earache or headache; painful urination; cold sores; and cuts or scrapes that are red, warm, swollen, or painful. If the patient is a carrier of the hepatitis B virus, Blitzima can cause the virus to become active. Hepatitis B can cause serious liver problems, including liver failure and death.
Progressive Multifocal Leukoencephalopathy (PML) and enteroviral meningoencephalitis
PML and enteroviral meningoencephalitis are very rare, serious brain infections that are caused by a virus. Individuals with weakened immune systems have an increased risk of infection. Symptoms of PML include confusion, memory loss, dizziness or loss of balance, difficulty walking or talking, weakness on one side of the body, and vision problems, and may be fatal. Symptoms of enteroviral meningoencephalitis include fever, headache, stiff neck, incoordination, personality changes, hallucinations, altered consciousness, seizures, and coma, and may be fatal.
Tumor Lysis Syndrome (TLS)
TLS is caused by the rapid breakdown of cancer cells. TLS can cause kidney failure. Symptoms of TLS include nausea, vomiting, diarrhea, and lack of energy.
Heart-related problems
Blitzima can cause a number of heart-related problems, including life-threatening irregular heartbeats (arrhythmia), or a heart attack. Patients with a history of heart-related problems should be carefully monitored during and after Blitzima infusion.
For a more complete list of possible side effects, see the full prescribing information.
Additional Information
Manufacturer
Celltrion Healthcare Hungary
Approval
EMA
Links to drug websites
- Europe: https://www.ema.europa.eu/en/medicines/human/EPAR/blitzima
Last updated on August 8, 2025


