How is the drug name pronounced?
Ofatumumab (compound): Oh-fa-too-moo-mab
Arzerra: ar-ZAYR-uh
What cancer(s) does this drug treat?
Arzerra is approved for:
Chronic lymphocytic leukemia (CLL)
- Patients with chronic lymphocytic leukemia (CLL) who have additional conditions and cannot be treated with the chemotherapy drug fludarabine. In such cases, Arzerra is used in combination with the chemotherapy drug chlorambucil.
- Patients with previously treated chronic lymphocytic leukemia (CLL) whose cancer has since returned (relapsed). In such cases, Arzerra is used in combination with fludarabine and cyclophosphamide chemotherapy.
- Patients with chronic lymphocytic leukemia (CLL) who were previously treated with fludarabine and alemtuzumab, but whose cancer stopped responding to the treatment (refractory).
- Patients with advanced chronic lymphocytic leukemia (CLL) who were successfully treated with at least two different types of therapy and whose cancer has decreased or disappeared. In such cases, Arzerra is given as maintenance therapy to prevent the cancer from getting worse or coming back.
Limitations of Use
Age: The safety and efficacy of Arzerra has not been established in patients under 18 years of age.
Vaccinations: Live virus vaccinations (e.g. chickenpox or measles, mumps, and rubella (MMR)) prior to or during Arzerra treatment are not recommended.
Pregnancy/breastfeeding: The effects on the fetus or newborn have not been studied for pregnant or breast-feeding women being treated with Arzerra. The potential risk to the fetus or newborn must be carefully weighed compared to the treatment needs of the mother.
What type of immunotherapy is this?
- Cell-killing antibody
How does this drug work?
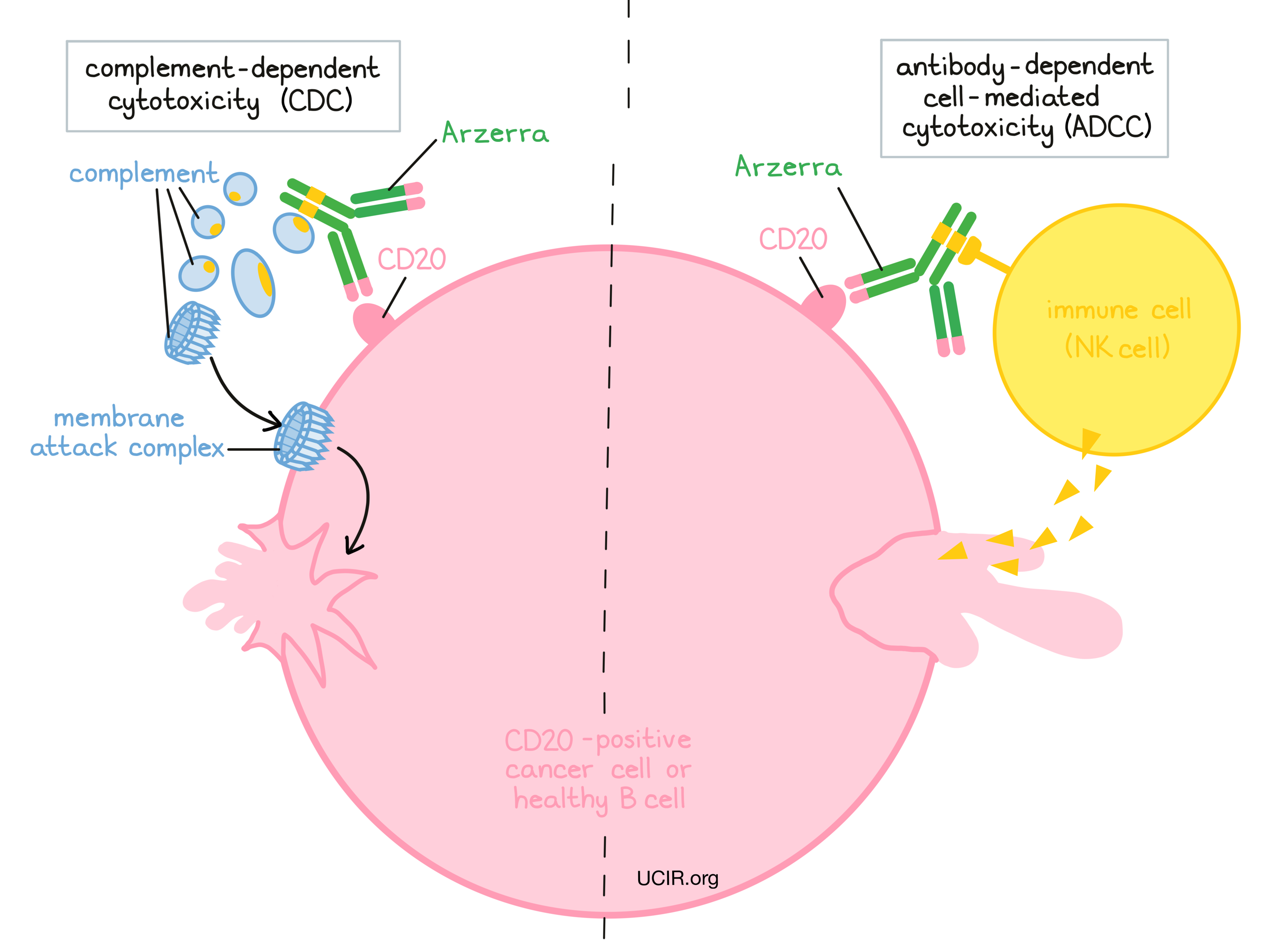
Target:
- CD20 molecule on B cells
Arzerra is an antibody that was made in the laboratory. Arzerra and other antibody molecules have an overall “Y” shape. The two tips of the upper arms of the “Y” shape are the parts of the antibody that can very precisely bind to their targets. Arzerra binds to a molecule called CD20 on the surface of a cancerous B cell. CD20 is commonly found on the surface of cancer cells in patients with chronic lymphocytic leukemia. CD20 can also be found on the surface of all normal human B cells, which means that in addition to attacking cancer cells, Arzerra can also attack healthy B cells.
The stem of Arzerra’s “Y” shape has binding sites for immune cells or other parts of the immune system.
Two different mechanisms are thought to be primarily responsible for the elimination of CD20-positive B cells by Arzerra. Arzerra is helped by the immune system to kill cancer cells.
Complement-dependent cytotoxicity (CDC)
When bound to CD20 on the surface of cancerous or normal B cells, the “stem” of Arzerra can attract and bind molecules of the immune system called “complement” that freely flow in the blood or tissues. Activation of the complement system causes the formation of the “membrane attack complex”, which can puncture and destroy the cell that Arzerra is bound to.
Antibody-dependent cell-mediated cytotoxicity (ADCC)
When bound to CD20 on the surface of cancerous or normal B cells, the “stem” of Arzerra can also attract and bind immune cells (like NK cells). This allows Arzerra to act as a bridge between the target cell and the immune cell. The immune cell then releases molecules that can kill the cell Arzerra is bound to.
The combined effect of these mechanisms results in the elimination of cancerous and normal B cells from the body. A new population of healthy B cells can then develop from blood-forming “stem cells” that reside in the bone marrow.
How is this drug given to the patient?
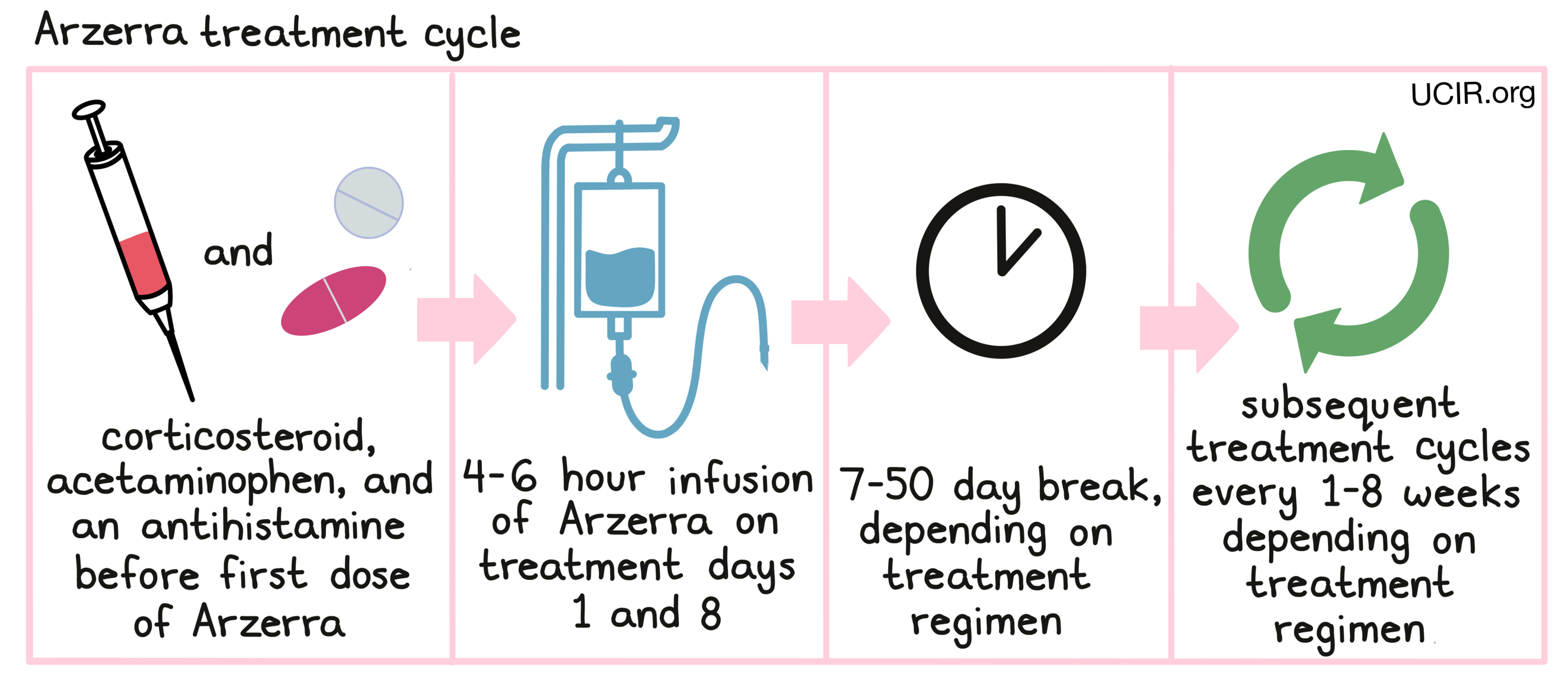
Arzerra is administered through a tube in the vein (intravenous infusion, or I.V.) every 1, 4, or 8 weeks. Each 1, 4, or 8 week period is one “treatment cycle”. The number of treatment cycles, the duration of treatment, and the dosage of Arzerra depends on the patient’s cancer.
The first treatment with Arzerra is usually given at a lower dose and may be followed up 1 week later with the standard dose. For all treatments, infusions will be initiated at a low rate, which may be increased every 30 minutes. In the absence of any serious side effects or reactions, a complete infusion of Arzerra can generally be expected to take anywhere from 4-6 hours. Administration of Arzerra does not require a hospital stay.
Before starting Arzerra therapy, patients will need to get blood tests done to check if the patient is a carrier of the hepatitis B virus. Arzerra can cause the virus to become active again, and patients who test positive for the hepatitis B virus will need to be monitored more closely during treatment and for several months afterward. Blood tests are also used to obtain complete blood counts on a regular basis during treatment and after ending treatment. This is because reductions in the number of blood cells are particularly common in patients being treated with Arzerra.
Prior to the first infusion and, if indeed, subsequent infusions, the patient will receive
- a corticosteroid, such as prednisolone, intravenously,
- acetaminophen by mouth, and
- an antihistamine such as diphenhydramine or cetirizine by mouth or intravenously
in order to reduce the risk of infusion-related side effects. If symptoms of an infusion-related reaction occur at any point during the first infusion or any subsequent infusions, the infusion may be interrupted or slowed, depending on the severity of the reaction. It is important that patients discuss with their doctor if they notice any changes following an Arzerra infusion, as infusion-related reactions are very serious.
What are the observed clinical results?
For:
Chronic lymphocytic leukemia (previously untreated)
Chronic lymphocytic leukemia (relapsed)
Chronic lymphocytic leukemia (refractory)
Chronic lymphocytic leukemia (maintenance treatment)
It is important to keep in mind that each patient’s actual outcome is individual and may be different from the results found in the clinical studies. In addition, with immunotherapy, sometimes it takes several months for responses to be observed.
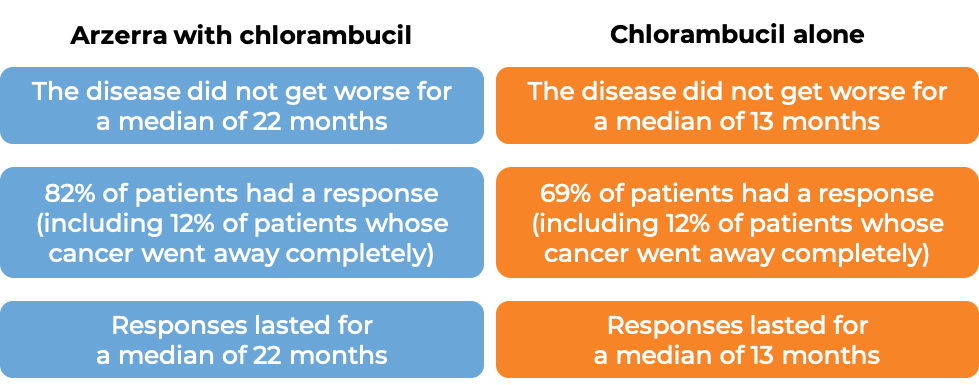
Chronic lymphocytic leukemia (previously untreated)
In a clinical study of 447 chronic lymphocytic leukemia (CLL) patients who could not be treated with the chemotherapy drug fludarabine because of advanced age or other medical conditions, patients were treated with either Arzerra in combination with chlorambucil, or with chlorambucil alone. At a median follow-up of 29 months:
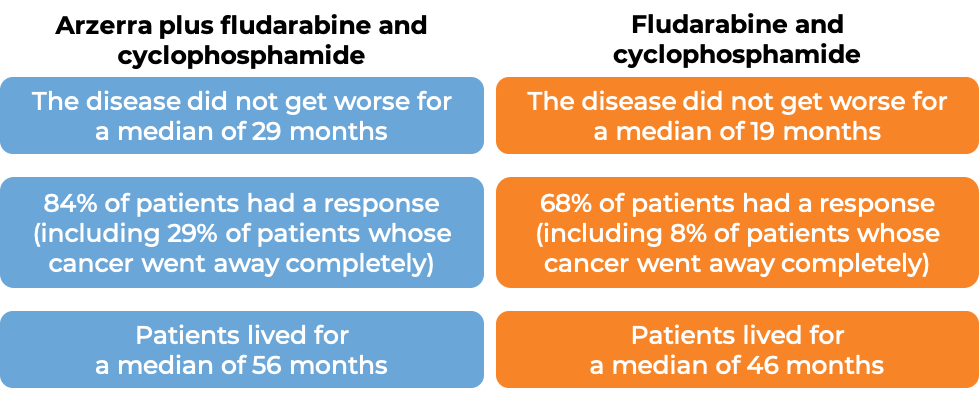
Chronic lymphocytic leukemia (relapsed)
In a clinical study of 365 chronic lymphocytic leukemia (CLL) patients who had been previously treated, but whose cancer had since returned (relapsed), patients were treated with either Arzerra in combination with fludarabine and cyclophosphamide, or with fludarabine and cyclophosphamide only. At a median follow-up of 34 months:
Chronic lymphocytic leukemia (refractory)
In a clinical study of 59 patients with chronic lymphocytic leukemia (CLL) who were previously treated with fludarabine and alemtuzumab, but whose cancer stopped responding to the treatment (refractory), patients were treated with Arzerra. Following treatment with Arzerra the extent of the cancer was reduced for 42% of the patients. There were no patients whose cancer went away completely. Responses lasted for a median of 7 months.
Chronic lymphocytic leukemia (maintenance treatment)
In a clinical study of 474 patients with advanced chronic lymphocytic leukemia (CLL) whose disease went away completely or was reduced after having 2 or more different types of treatment, patients were either treated with Arzerra or not treated (observation). Patients treated with Arzerra lived without their disease getting worse for a median of 29 months, compared to 15 months for patients in the observation group. At a median follow-up of 19 months, 67% of patients were alive and had no worsening of their disease, compared to 49% of patients under observation.
What are the potential side effects?
Arzerra targets the CD20 molecule, which, while present on leukemic B cells, is also present on normal B cells. As a result, Arzerra can kill normal B cells, increasing the risk of serious infections and sepsis, including respiratory infections. Arzerra may also cause reactivation of the Hepatitis B Virus (HBV). Other common side effects of Arzerra include low blood cell counts (particularly low counts for infection-fighting neutrophils), skin rashes, insomnia, headache, back pain, weakness, nausea, fever, cough, diarrhea and cardiac issues such as elevated heart rate and high or low blood pressure.
Some side effects, such as reactions related to the infusion, severe infections, infections of the brain, hepatitis B virus reactivation, tumor lysis syndrome, heart problems, and kidney problems, may be severe or life-threatening. Patients and caregivers receive careful instructions to monitor for signs and symptoms of these complications, and a healthcare provider should be immediately notified if symptoms occur. These conditions are managed by a health care provider.
Infusion-related reactions
Reactions to the Arzerra infusion are common. Some of these reactions are serious. Symptoms include hives, rashes, swelling of lips, tongue, or face, sudden cough, shortness of breath, difficulty breathing, dizziness or feeling faint, heart racing or fluttering, and chest pain.
Serious infections and hepatitis B virus reactivation
Arzerra can reduce the immune system’s ability to fight off bacterial, fungal, and viral infections, can increase a patient’s risk of getting an infection, and can cause the reactivation of prior viral infections. These infections can be serious, and may be fatal. Symptoms of infection include: fever; cold symptoms, such as a persistently runny nose or sore throat; flu symptoms, such as coughing, tiredness, and achiness; earache or headache; painful urination; cold sores; and cuts or scrapes that are red, warm, swollen, or painful. If the patient is a carrier of the hepatitis B virus, Arzerra can cause the virus to become active. Hepatitis B can cause serious liver problems, including liver failure and death.
Tumor Lysis Syndrome (TLS)
TLS is caused by the rapid breakdown of cancer cells. TLS can cause kidney failure and abnormal heart rhythms. Symptoms of TLS include nausea, vomiting, diarrhea, and lethargy.
Progressive Multifocal Leukoencephalopathy (PML)
PML is a rare, serious brain infection that is caused by a virus. Individuals with weakened immune systems have an increased risk of infection. Symptoms of PML include confusion, dizziness or loss of balance, difficulty walking or talking, weakness on one side of the body, and vision problems.
For a more complete list of possible side effects, see the full prescribing information.
Additional information
Manufacturer
Novartis
Approval
FDA
Links to drug websites
- US: https://www.us.arzerra.com/
Last updated on October 5, 2020


