Cancer care in the age of COVID-19
2021-02-26
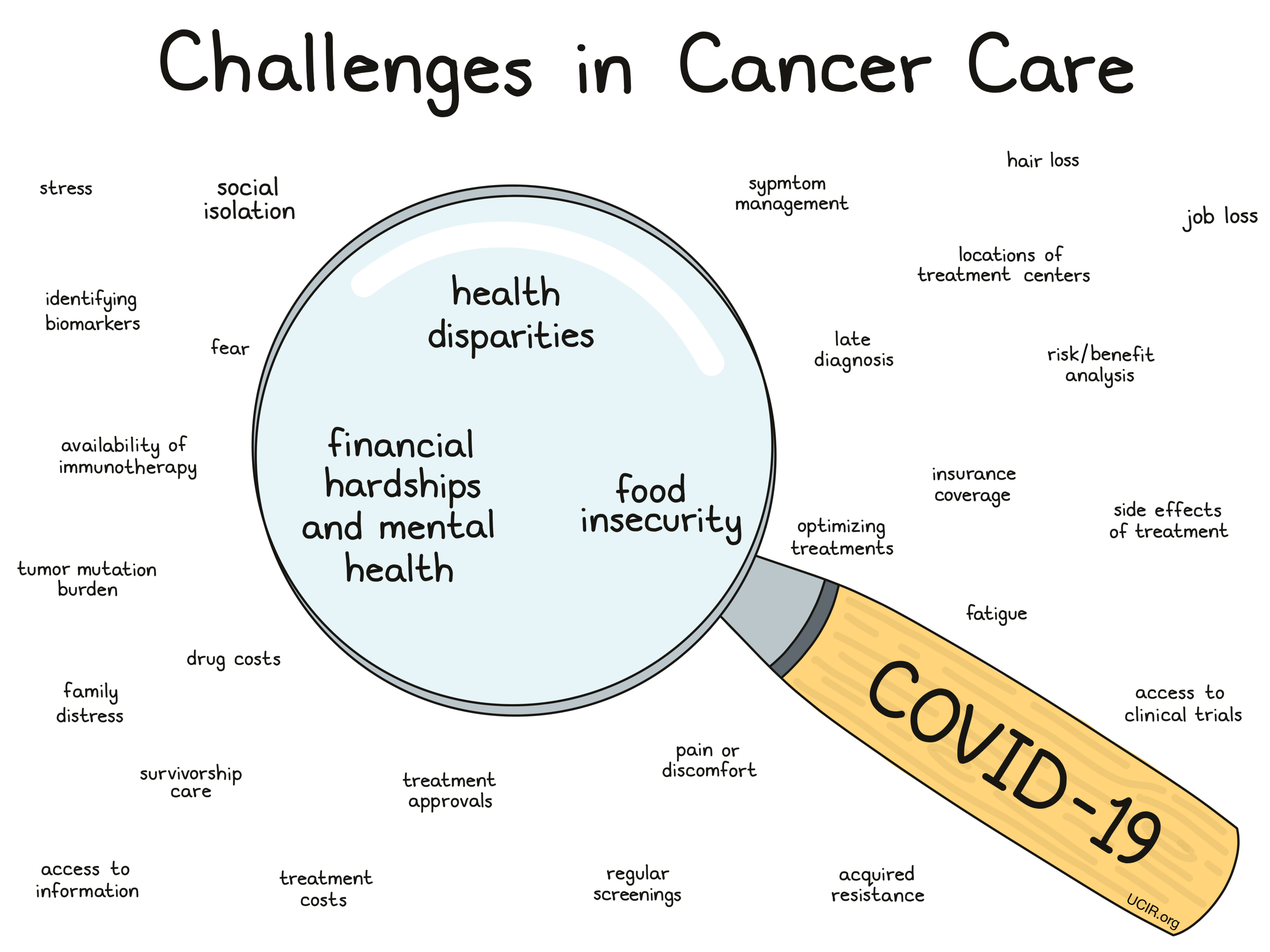
When the COVID-19 pandemic struck the world, routines of all kinds were uprooted, and cancer testing and care were no exception. Settling into the new normal, there are many new challenges involved in cancer treatment that demand immediate and long-term solutions. UCIR recently attended the AACR-sponsored virtual meeting “COVID-19 and Cancer” February 3-5, 2021 to better understand these issues.
Challenge: Finding ways for patients see their doctors safely
First and foremost, the most obvious challenge of the COVID-19 pandemic is reducing the risk of contracting and spreading COVID-19. While staying home and social distancing have helped to curb the spread of COVID-19, these same measures have kept patients away from their doctor’s offices, which has led to missed appointments, reduced routine screenings, fewer cancer diagnoses, and delayed cancer treatment, all of which can lead to worse clinical outcomes. Moving forward, it is important to weigh the risks associated with COVID-19 against the risks associated with cancer progression. Overall, there is a major need to get patients back on track so that cancer can be diagnosed, treated, and followed up on appropriately.
Solutions: One way that many patients are now seeing their doctors is through telehealth. While these phone or video calls with doctors cannot replace all in-person care, they are a good way for many patients to speak with their doctors and determine if an in-person visit is necessary. Similarly, telehealth allows doctors to prescribe medications, which can even be set up for home delivery, reducing the need for pharmacy visits. In some cases, oral prescriptions that can be taken at home may be able to replace certain medications that would be delivered by IV injection in a hospital setting. When patients do require in-person visits, it is important that healthcare facilities have COVID-19 safety protocols in place and that patients follow those protocols. Further, some have suggested that all patients with cancer and survivors should be vaccinated as early as possible, regardless of whether their cancer puts them at a high risk for severe COVID-19 infection, so that they are able to safely receive the in-person cancer care they need. In fact, 130 cancer-focused institutions recently signed a letter, initiated by the AACR, to United States President Joe Biden and other key members of his administration urging federal and state health officials to give priority access to a COVID-19 vaccine for active patients and survivors of cancer.
_______________________________________________________________________________________________
Challenge: Screening for and diagnosing cancer
The COVID-19 pandemic has greatly reduced patients’ attendance at regular doctor’s visits and routine screenings for certain cancers. Screenings for breast and colon cancer were down by as much as 94% during the early months, but have at least partially recovered. Routine screenings can catch cancers early, and without them, cancers may progress in patients undetected, leading to later diagnoses and poorer chances of survival. Many healthcare facilities still do not yet have the resources to return to regular screenings at full capacity, and patients may not yet feel comfortable returning for them, so there is a new need for alternative screening and diagnostic strategies.
Solutions: One possible strategy to improve cancer screening in the COVID-19 pandemic would be to use “risk assessment” methods to determine which patients are the highest priority for cancer screening. Taking into account prior cancers, family history, behaviors, age, and various other risk factors may allow for patients with the highest risk of cancer to be screened first. For some cancers, like colorectal cancer, at-home testing options are available and may help to flag patients who have markers of disease or are at high risk for disease, so that those patients can be brought in for further testing.
_______________________________________________________________________________________________
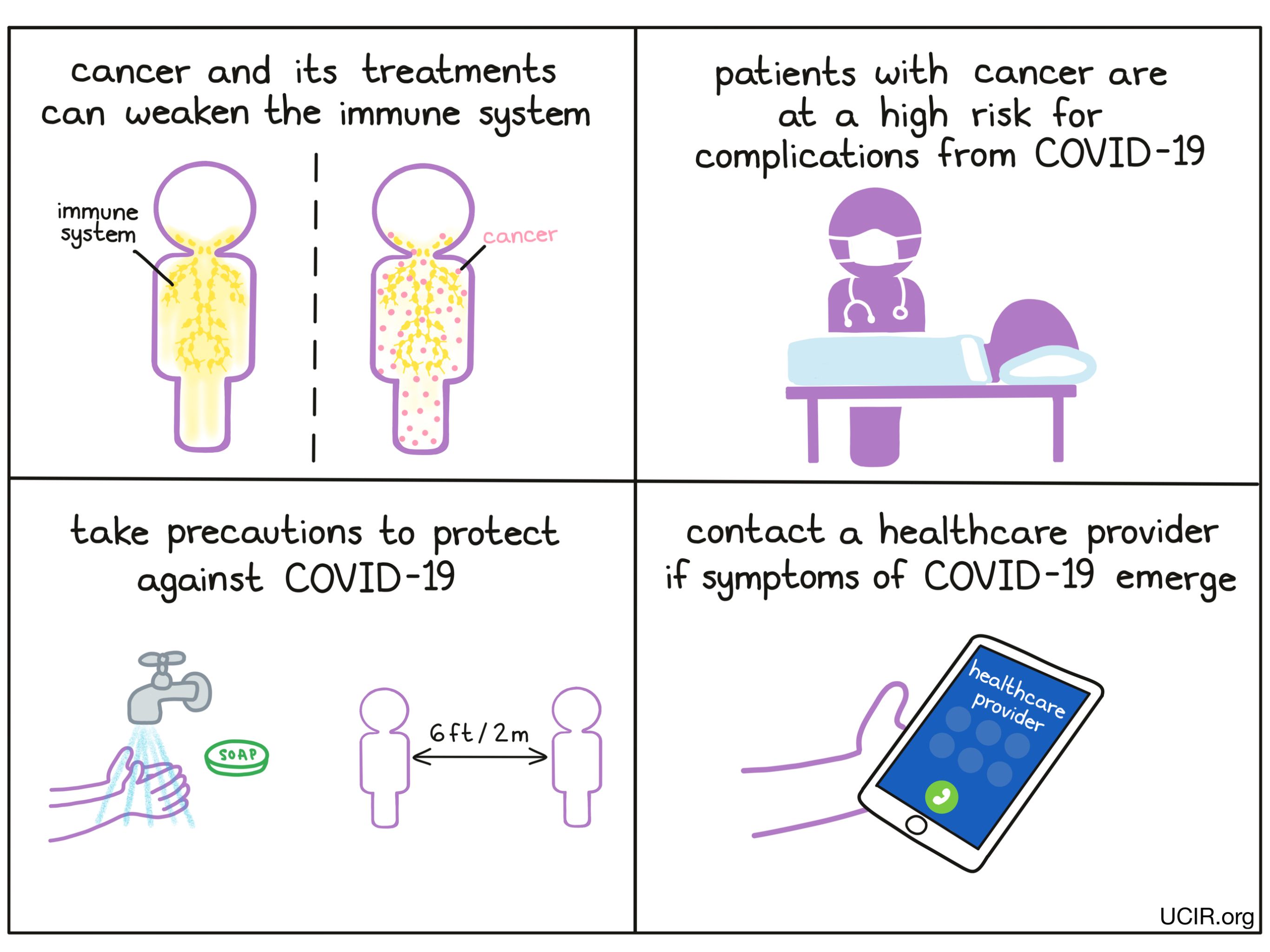
Challenge: Treating COVID-19 infections in patients with cancer
Unfortunately some patients with cancer may also contract COVID-19. Several cancers or their therapies may increase the risk for severe COVID-19, while other cancers may be a less significant risk factor. Therapies that temporarily compromise the immune system are particularly problematic. In certain cases, COVID-19 infection may resemble symptoms of cancer or side effects of cancer treatments, and it may be difficult to distinguish which is which.
Solutions: Further investigations are necessary to determine which cancers are most likely to increase the risk for COVID-19 infections or the severity of those infections. It may also be useful for patients to be tested for COVID-19 before, during, and after treatment in order to distinguish symptoms. It will also be important to explore whether COVID-19 infection should be a factor in delaying certain cancer treatments. Doctors will need to compare the risks of severe COVID-19 infection with the risks of cancer progression if treatment is withheld.
_______________________________________________________________________________________________
Challenge: Reaching vulnerable patient populations
Certain populations of patients can be hard to reach in the best of times, and with the COVID-19 pandemic, these patients are facing even more hurdles in accessing care. Older patients are struggling with telehealth technologies, certain racial populations have lost trust in the healthcare industry, and the number of patients with low incomes or who are uninsured has skyrocketed in the face of unprecedented job loss. In addition to these populations being at a higher risk for COVID-19, these patients are being chronically underserved in the field of cancer care, and efforts to reach them need to be amplified.
Solutions: In order to reach vulnerable patient populations, there is a need for reinvigorated efforts to establish outreach programs that build trust with facilities and providers. Cancer screening and cancer care need to be made affordable and accessible to patients in vulnerable, high-risk populations. Providing information to patients at drive-through testing or vaccination sites in high-risk communities may help to reach patients who might not otherwise be inclined to seek testing or care for cancer.
_______________________________________________________________________________________________
Challenge: Addressing the mental, emotional, and social needs of patients with cancer through COVID-19
Cancer is a physical disease, but it also puts serious emotional, social, and financial burdens on patients and their families. In the age of COVID-19, these burdens may be amplified, as many patients and families struggle with social isolation, caring for children at home, job loss, loss of health insurance, and more. Patients with cancer do better when they have strong social and emotional support systems in place, and there is a need to adjust support networks to accommodate new issues that are not directly related to healthcare.
Solutions: While in-person interactions should remain limited through the COVID-19 pandemic, it is important to encourage patients to maintain social connections with family and friends as best they can. Encouraging healthy behaviors at home, including exercise and eating well, may also help patients. Further, it could be beneficial to establish more home-based programs that help patients and survivors connect with one another and build supportive virtual communities. Video conferencing with mental health care providers could also be useful.
_______________________________________________________________________________________________
Challenge: Decreased enrollment in clinical trials
The COVID-19 pandemic has created unique challenges for patient enrollment in clinical trials for new cancer therapies, including novel immunotherapies. On the clinical side, many trials were temporarily stopped during the earliest peak of the pandemic. Additionally, many have been delayed or slowed due to lack of funding, reallocation of resources and staff, reduced access to labs and radiology, and in some cases, certain drugs or treatments were withheld for fear that they might increase the risk for severe COVID-19 infection. On the patient side, enrollment in clinical trials has also decreased, potentially due to social distancing measures, travel restrictions, or reduced access to support from family and friends. This delays the progress of potential new cancer therapies, as new drugs and protocols need to be tested in clinical trials before they can become more widely available.
Solutions: While most cancer treatment still requires in-person care, some preliminary and follow-up appointments can potentially be managed through virtual visits and telemedicine, reducing a patient’s need to travel to participate in a clinical trial. Some drugs could potentially be shipped to patients, and at-home testing could allow patients to take some samples remotely and mail them in for laboratory testing, or routine tests could be done at more conveniently located testing facilities. As far as designing clinical trials is concerned, utilizing shorter treatment schedules, selecting oral treatment options over IV, and avoiding treatments that include immunocompromising medications would be prudent.
_______________________________________________________________________________________________
Challenge: Reduced funding for cancer research
COVID-19 is at the top of everyone’s minds… and wallets. With loads of funding being redirected towards COVID-19 research, there is less to go around for other organizations, including those centered around cancer research and cancer care. The need for cancer research and cancer care has not gone away during the COVID-19 pandemic, and if anything, there is a demand for more funding than ever to support newer, safer ways of providing care in a healthcare system that is rapidly adjusting to the new normal.
Solutions: There needs to be a renewed push for funding through grants, corporate donations, and private donations to support the financial needs of cancer research institutions, hospitals, and patients. COVID-19 is deadly, but so is cancer, and there needs to be enough funding and resources available in order to save lives on both fronts.
_______________________________________________________________________________________________
Conclusion:
While COVID-19 has changed the landscape of cancer care, this field is known for overcoming challenges. There is still room to adapt and change in order to get cancer care back on track, and by pursuing creative solutions and assessing them with a critical eye, it may soon be possible to resume cancer care as we knew it and upgrade to even better systems and strategies to safely diagnose, treat, and cure cancer in as many patients as possible.
Write-up by Lauren Hitchings
References:
Talks presented at the “AACR COVID-19 and Cancer” conference February 3-5, 2021:
Challenges to cancer screening during the COVID-19 pandemic
Mary E. Reid, Roswell Park Comprehensive Cancer Center, Buffalo, NY
Breast cancer screening during the COVID-19 pandemic: Are we ready for a risk-based approach?
Katherine D. Crew, Columbia University, New York, NY
Long-term effects and impact of COVID-19 pandemic on cancer survivorship
Larissa Nekhlyudov, Brigham and Women’s Hospital/Dana-Farber Cancer Institute, Boston, MA
Effects of demographic and behavioral factors on social isolation in a cancer center population during COVID-19 pandemic
Shelley Tworoger, Moffitt Cancer Center, Tampa, FL
Impact of the COVID-19 pandemic on social and health behaviors among rural and urban cancer patients at Huntsman Cancer Institute (HCI)
Bailee Daniels, Huntsman Cancer Institute, Salt Lake City, UT
Impact of the COVID-19 pandemic on oncology care delivery: From screening to surveillance
Trisha Wise-Draper, University of Cincinnati, Cincinnati, OH
Disruption to care of patients with thoracic malignancies: A COVID-19 and cancer outcomes study
Sheena Bhalla, Icahn School of Medicine at Mount Sinai, New York, NY
Telehealth experiences of adolescent and young adult cancer patients and survivors during the COVID-19 pandemic
Karely Mann, Huntsman Cancer Institute, Salt Lake City, UT
Recommendations supporting continuity of care: Landscape, perspectives, limitations, and open questions
Giuseppe Curigliano, University of Milan, Milan, Italy